
Key Points (These points are a summary of each of the research studies that are presented at the end of this document):
For up to date information regarding COVID & pregnancy, we recommend visiting Evidence Based Birth here. On their site, you can also download their free printable handout on the Evidence on COVID-19 Vaccines in Pregnancy.
January 2, 2021 – Since 2016, the total number of registered deaths in the United States ranged from 2.75 to 2.85 Million, as reported by the CDC (see references below). As of January 2, total registered deaths have only been officially reported on the CDC website for the first six months of 2020. If the trend is accurate (and it may not be), indications are that the United States may ultimately report as many as 3.25 Million registered deaths, an increase that is significantly higher than what would otherwise be expected. This would seem to indicate that regardless of whether or not Covid is receiving unfair “credit” for whichever illness that people are dying from, there are still an extraordinary amount of deaths compared to usual.
January 2, 2021 – The concept of vaccines: to expose your system to a less aggressive version of any particular virus, in hopes that your immune system will intelligently develop a counter-attack that can more effectively be employed if ever you come in contact with the full strength of the virus. There are several ways that this exposure is achieved, ranging from using dead viruses, to parts of the virus, and now even to tiny genetic samples of the virus. In order to achieve these less-aggressive forms of the virus, various additional ingredients are often used. Side effects from vaccines can occur due to the virus itself, but also due to the other ingredients in the vaccine. Regardless your decision about vaccination, bolstering your Five Foundations is the powerful foundation of your wellness: (Breathing, Movement, Nutrition, Lifestyle and Thoughts). (Learn how to strengthen your 5 Foundations during pregnancy, here!)
December 8, 2020 – “Numerous vaccines are being evaluated in clinical trials, but pregnant and lactating individuals have been excluded from every trial.” – Evidence Based Birth, email sent Dec. 8, 2020, titled, “Research Update on COVID-19 and Pregnancy: Special Edition on Vaccines”
September, 2020 – Infants born to mothers with SARS-CoV-2 did NOT suffer any additional adverse outcomes (areas tested included preterm birth, NICU admission, respiratory disease, low birth weight, difficulty breathing, apnea or upper or lower respiratory infection.)
August, 2020 – Because of the importance of growth, development and bonding, mothers and infants are recommended to be kept together whenever safely possible. It is also recommended to acknowledge the potential psychological distress that may be present during this time; to promote women’s control and choice whenever possible; and to use a collaborative approach to ensure that mental, physical, emotional, and social needs are being met.
June, 2020 – Coronavirus infection can cause higher risk of some symptoms in pregnant women (like viral pneumonia) which can, in turn, affect the fetus’ health (for example hindering intrauterine growth or complicating intestinal function). However, the disease condition in most children has proven mild thus far.
June, 2020 – Pregnant women with COVID are more likely to need hospitalization and intensive care, compared to non-pregnant women with COVID
June, 2020 – Babies who are birthed vaginally, breastfeed and have contact with their mothers have no greater chance of contracting SARS-COV-2
June, 2020 – Undergoing a C-section – within the Covid-19 atmosphere – is associated with increased risk of postpartum maternal complications as well as infant’s need for intensive care
May, 2020 – Placentas of pregnant mothers who had COVID show physiological signs of subnormal oxygenation, however, since placentas are considerably over-proficient, the health of these babies are generally not compromised
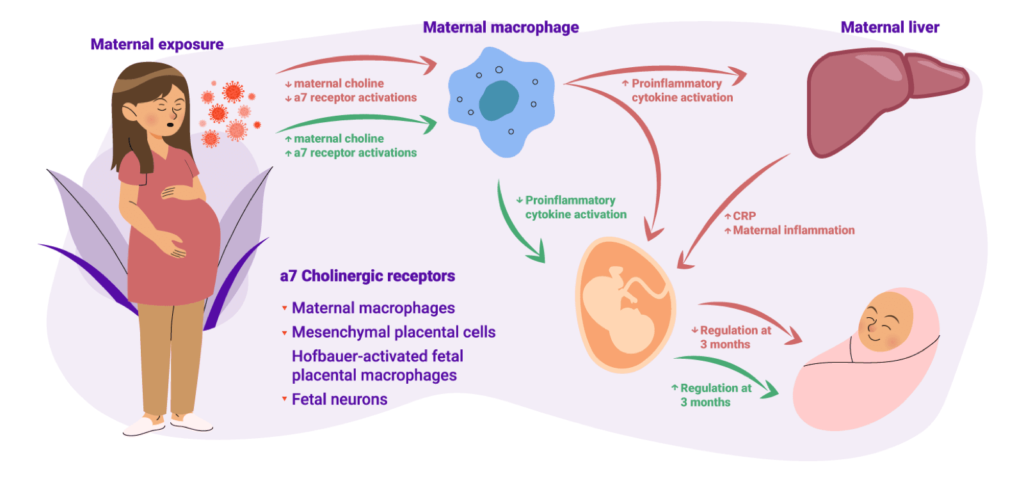
May, 2020 – The nutrient Choline may help pregnant women decrease negative effects on their babies
May, 2020 – Vitamin D determines severity of Covid-19 (aside from Covid, higher doses are recommended during pregnancy)
March, 2020 – “Quarantine” exercise still boosts immunity
The World Health Organization (WHO) explains why there are several terms given to the phenomenon that has been called “the event of our lifetime.” Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the virus that causes Coronavirus disease (COVID-19). The WHO says, “Viruses, and the diseases they cause, often have different names,” which is equivalent to HIV being the virus that causes AIDS.[1]

What follows are some details of the initial and most profound recent studies regarding pregnancy and postpartum amidst COVID.
January 2, 2021:Vaccines & COVID Discussion:
Total Number of Deaths in the United States, year by year (all CDC Stats):
- 2016 = 2.74M. 2,744,248.[2] //// (849.3 per 100,000)[3]
- 2017 = 2.81M. 2,813,503.[4] //// (731.9 per 100,000)[5]
- 2018 = 2.84M. 2,839,205.[6] //// (723.6 per 100,000)[7]
- 2019 = 2.85M. 2,854,838.[8],[9] //// (870.0 per 100,000? “crude”)[10]
- 2020: Jan-Jun, # of deaths are: 264k + 244k + 269k + 321k + 279k + 249k = 1.626M. Doubling this for the remainder of 2020 would = 3.25M
- As of Nov. 21, 2020, CDC website is using the 2018 number: 2,839,205.[11] (867.8 per 100,000)[12]
- CBS 19 Texas projection on October 3: 3.1M deaths in 2020[13]
- The information for 2016-2020 all come from the CDC website, as referenced in the footnotes. The total deaths registered for 2018 and 2019, for example, can be found very simply in reports titled “Mortality in the United States, 2018” and “Mortality in the United States, 2019.” However, as of January 2, 2021, there was no CDC report identifying: “Mortality in the United States, 2020”
Vaccines, According to EBB:[14]
- Vaccine safety trials began in March, 2020. According to NY Times Vaccine Tracker, there are 58 human vaccine trials. 13 have reached final stages of testing. 7 have been approved for early or limited use.
- “Numerous vaccines are being evaluated in clinical trials, but pregnant and lactating individuals have been excluded from every trial.”

Types of COVID Vaccines:
Genetic Vaccine/ mRNA technology
- EBB: “The newest technology being used to develop coronavirus vaccines are genetic vaccines that use messenger RNA (mRNA) technology. These vaccines deliver one or more of the coronavirus’ genes into human cells to stimulate immunity. Pfizer/BioNTech and Moderna are developing mRNA vaccines. In many countries around the world, including in the U.S. and the U.K., these mRNA vaccines are going to be the first ones available.”
- “Gene vaccines are a new approach to immunization and immunotherapy in which, rather than a live or inactivated organism (or a subunit thereof), one or more genes that encode proteins of the pathogen are delivered.”[15] [2003]
- “…messenger RNA technology, which prompts the body to make a key protein from the virus, creating an immune response.”[16]
- [Nov. 24, 2020] – “Within the next month, messenger RNA vaccines—also called mRNA vaccines—are likely to be some of the first COVID-19 vaccines authorized for use in the United States…mRNA vaccines take advantage of the process that cells use to make proteins in order to trigger an immune response and build immunity to SARS-CoV-2, the virus that causes COVID-19. In contrast, most vaccines use weakened or inactivated versions or components of the disease-causing pathogen to stimulate the body’s immune response to create antibodies…mRNA vaccines have strands of genetic material called mRNA inside a special coating. That coating protects the mRNA from enzymes in the body that would otherwise break it down. It also helps the mRNA enter the muscle cells near the vaccination site. mRNA can most easily be described as instructions for the cell on how to make a piece of the “spike protein” that is unique to SARS-CoV-2. Since only part of the protein is made, it does not do any harm to the person vaccinated but it is antigenic.After the piece of the spike protein is made, the cell breaks down the mRNA strand and disposes of them using enzymes in the cell. It is important to note that the mRNA strand never enters the cell’s nucleus or affects genetic material. This information helps counter misinformation about how mRNA vaccines alter or modify someone’s genetic makeup. Once displayed on the cell surface, the protein or antigen causes the immune system to begin producing antibodies and activating T-cells to fight off what it thinks is an infection. These antibodies are specific to the SARS-CoV-2 virus, which means the immune system is primed to protect against future infection.”[17]
EBB: “Some traditional vaccines, such as those used for the seasonal flu, polio, and hepatitis A, use inactivated (killed) virus. Several inactivated viruses are being developed and four are in Phase 3 trials (three from China and one from India). There are also attenuated (weakened) virus vaccines in development, but none are in Phase 3 trials yet.”
- Inactivated Vaccines – “There are several types of vaccines that can be used to fight diseases. Inactivated vaccines are composed of dead, or inactivated, viruses and bacteria, and therefore differ from live but attenuated vaccines.”[18]
- Live Attenuated Vaccines – strong>“Advances in tissue culture techniques in the 1950s enabled development of live-attenuated vaccines, which contain a version of the living microbe that has been weakened in the laboratory.”[19] “Many vaccines that are regularly used, such as the MMR vaccines and chickenpox vaccines, are live attenuated vaccines. These vaccines have a weakened version of the live virus, to stop it from causing the disease but to still encourage the production of T cells. Inactivated vaccines are another form of vaccine, where the virus is inactivated during the process of making the vaccine…Because the virus is dead during the making of the vaccine, they interact with the immune system differently than live, attenuated vaccines. The immune response to live vaccines is similar to encountering the virus itself, whereas inactivated vaccines show little or no cellular immunity. ”[20]
Viral Vector Vaccines – [July, 2019] –
- BB: “Viral vector vaccines are newer technology. With these, a SARS-CoV-2 gene for the spike protein is inserted into another virus (often an adenovirus) to deliver the gene to human cells. Then, the production of surface spike protein causes the immune system to recognize the virus if infected. AstraZeneca and Johnson & Johnson are both developing their COVID-19 vaccines using the viral vector approach.”
- “Recombinant vector vaccines are live replicating viruses that are engineered to carry extra genes derived from a pathogen—and these extra genes produce proteins against which we want to generate immunity. These vaccine genomes may evolve to lose the extra genes during the process of manufacture of the vaccine or during replication within an individual, and there is a concern that this evolution might severely limit the vaccine’s efficacy.”[21]
- “Adenovirus vectors deliver the genetic instructions for SARS-CoV-2 antigens directly into patients’ cells, provoking a robust immune response. …Six vaccine candidates in clinical trials for COVID-19 employ viruses to deliver genetic cargo that, once inside our cells, instructs them to make SARS-CoV-2 protein. This stimulates an immune response that ideally would protect recipients from future encounters with the actual virus….. Three candidates rely on weakened human adenoviruses to deliver the recipe for the spike protein of the pandemic coronavirus, while two use primate adenoviruses and one uses measles virus. Once inside a cell, viral vectors hack into the same molecular system as SARS-CoV-2 and faithfully produce the spike protein in its three dimensions. This resembles a natural infection, which provokes a robust innate immune response, triggering inflammation and mustering B and T cells. But the major downside to the human adenoviruses is that they circulate widely, causing the common cold, and some people harbor antibodies that will target the vaccine, making it ineffective.”[22]
- ““The problem with adenovirus vectors is that different populations will have different levels of immunity, and different age groups will have different levels of immunity,” says Nikolai Petrovsky, a vaccine researcher at Flinders University in Australia.”[23]
- “One of the key biological characteristics of SARS-CoV-2, as well as several other viruses, is the presence of spike proteins that allow these viruses to penetrate host cells and cause infection…. the S protein plays a crucial role in penetrating host cells and initiating infection…Notably, the presence of S proteins on the coronaviruses is what gives rise to the spike-shaped protrusions found on their surface…Without the S protein, viruses like the novel SARS-CoV-2 would never be able to interact with the cells of potential hosts like animals and humans to cause infection. As a result, the S protein represents an ideal target for vaccine and antiviral research endeavors.”[24]

Viral Vector Vaccines – [July, 2019] –
- EBB: “Other traditional vaccines, such as those used for pertussis and hepatitis B, use a part of the virus (typically one or more proteins) to trigger an immune response. In the case of COVID-19 vaccines, they would use the spike protein on the surface of the virus—these are sometimes called protein-based vaccines”
- “Protein based subunit vaccines present an antigen to the immune system without viral particles, using a specific, isolated protein of the pathogen. A weakness of this technique is that isolated proteins, if denatured, may bind to different antibodies than the protein of the pathogen.”[25]
According to EBB, email sent Dec. 8, 2020, titled, “Research Update on COVID-19 and Pregnancy: Special Edition on Vaccines”:
Vaccine efficacy seems to show a reduction in “symptomatic COVID-19”
What is in a Vaccine & Why? [CDC; Aug 5, 2019][26]
- Preservatives, like Thimerosal, to prevent contamination
- Adjuvants, like Aluminum salts, to help boost the body’s response to the vaccine
- Stabilizers, like sugar & gelatin, to keep the vaccine effective after manufacturing
- Residual Cell Culture Materials, like egg protein, to grow enough of the virus or bacteria to make the vaccine
- Residual Inactivating Ingredients, like Formaldehyde, to kill viruses or inactivate toxins during the manufacturing process
- Residual Antibiotics, like Neomycin, to prevent contamination by bacteria during the vaccine manufacturing process
Three examples:
Pfizer/BioNTech – 43,000 participants. Symptomatic Covid in 162 placebo but only 8 in the vaccine group.
- “BioNTech received $445 million from German government”[27]
Moderna – 30,000 participants. 185 “cases” of COVID in the placebo group but only 11 in the vaccine group. (30 severe cases, all in the placebo group).
- “Moderna vaccine funded by government spending, with notable private donation” [USA Today]
- “The New England Journal of Medicine recognized support from Emory University, Vanderbilt University Medical Center, the Dolly Parton COVID-19 Research Fund and other organizations”
AstraZeneca/University of Oxford Vaccine – 30,000 participants. 101 “cases” of COVID in the placebo group, but only 30 in the Vaccine group. (Zero “severe cases” in the vaccine group)
- “AstraZeneca has received more than $1 billion from the U.S. Health Department’s Biomedical Advanced Research and Development Authority to develop a coronavirus vaccine from the University of Oxford.”[28]
Adverse effects so far seemed to include:
- “fatigue (3.8%) and headache (2%). ‘Severe’ side effects were defined in the study protocol as those that prevent ‘daily routine activity.’ We could not find additional info about side effects in the company’s press releases”
- “…injection site pain, fatigue, muscle aches and pains, joint pain, headache, and redness at the injection site… adverse reactions increased in frequency and severity in the vaccine group after the second dose.”
SOME OF THE EVIDENCE BASED BIRTH “WE DON´T KNOW´S”:
- We don’t know if the vaccines actually prevent transmission of COVID
- We don’t know how long vaccine-induced immunity lasts.
- We don’t know the long-term safety concerns of the vaccines.
- We don’t know how the virus will evolve, making the vaccines less effective.
The CDC itself has identified areas where government agencies did not properly regulate various medicines, and as a result, subsequent damage and lawsuits have occurred as a result of this corruption (check the stories of Semmelweis/Puerperal Fever and Diethylstilbestrol, as two examples). Therefore, we at Fit For Birth understand that for many of you, the evidence presented here, both from the CDC and especially within these vaccine studies is subject to speculation. Funding sources for the research studies, although listed above, have not been vetted by Fit For Birth to determine motive, health vs. profit, etc. In many cases, it isimpossible to determine motives until evidence appears later. Sometimes that evidence appears, and there are class-action lawsuits, but many times it does not. We know that vaccination is a super-charged topic for so many, and we sincerely wish you the guidance of Spirit in making your decisions for your pregnant body and your family.
SOME OF THE EVIDENCE BASED BIRTH “WE DON´T KNOW´S”:
- 1 Alignment- Aim to support the BELIEF of your client. Whatever she chooses, help her mind to “catch up to” feeling good about her choice.
- 5 Foundations- Now is the time for basic foundational health protocols!!!! Whether your client wants to avoid the adverse effects of taking the vaccine, or of not taking the vaccine, her body and her baby will be more able to manage if she has taken steps to strengthen her 5 Foundations!

September 18, 2020 – Clinical Infectious Disease[29] “Infant Outcomes Following Maternal Infection with SARS-CoV-2: First Report from the PRIORITY Study”
- “Among a U.S. registry of 263 infants born to mothers testing positive or negative for SARS-CoV-2…suspected or confirmed SARS-CoV-2 during pregnancy or in the first 6 weeks after pregnancy. This manuscript reports infant outcomes for live births occurring to 179 mothers who had a positive test for SARS-CoV-2 and 84 mothers who had a negative test for SARSCoV-2 and excludes live births of 10 mothers suspected of SARS-CoV-2 who were not tested. Maternal out
- Among those testing positive, 146 (81.6%) were symptomatic, while among those testing negative, 53 (63.1%) were symptomatic
- Among 263 initial infants enrolled in the PRIORITY study, adverse outcomes, including preterm birth, NICU admission, and respiratory disease did not differ between those born to mothers testing positive for SARS-CoV-2 and those born to mothers testing negative.
- SARS-CoV-2 status was not associated with birth weight, difficulty breathing, apnea or upper or lower respiratory infection through 8 weeks of age”
August 11, 2020 – Journal of Obstetric, Gynecologic & Neonatal Nursing (JOGNN)[30] “Promotion of Maternal–Infant Mental Health and Trauma-Informed Care During the COVID-19 Pandemic.” Addressing Mental Health of a pandemic during the perinatal period.
- “Emerging evidence suggests that pregnant women are at similar risk for contracting COVID-19 and have a comparable disease course to that of the general population, but the research is still evolving, and many unanswered questions about the effects of COVID-19 on childbearing women and infants remain, such as the long-term effects of COVID-19 on fetal development, infant development, and reproductive health (Liu et al., 2020; Qiao, 2020; World Health Organization [WHO], 2020; Yan et al., 2020). It is not yet known whether the virus can be transmitted to a fetus during pregnancy or to an infant during birth and breastfeeding (Schwartz et al., 2020; WHO, 2020; Yan et al., 2020).
- Although current evidence remains insufficient to suggest that there is greater risk for severe COVID-19 illness for pregnant women than the general population, there is consensus among these organizations that careful infection control precautions are warranted, given the many unknowns about COVID-19 and pregnancy.
- During the pandemic, women are at increased risk for depression, anxiety, posttraumatic stress disorder, and suicidality precipitated by new pandemic-related stressors (Thapa et al., 2020). These negative mental health effects may occur as a result of distress from infection or hospitalization of family members; traumatic loss and bereavement from COVID-19 deaths; increased caregiving demands for children and family members who are spending more time at home; isolation from community due to social distancing, job loss, and financial hardship related to closure of nonessential businesses; increased interpersonal stressors or relationship violence secondary to pandemic stressors; and uncertainty about the future (Shah et al., 2020). The short- and long-term psychological effects of the pandemic have the potential to disproportionately harm women from marginalized and under-resourced communities. These may include underrepresented minority communities in which there is strong evidence of disparities in rates of infection and mortality, communities with undocumented immigrant residents, communities with limited access to technology and health care resources, and communities that experience housing instability or homelessness (Gross et al., 2020).”
- Regarding childbearing women, “Previous pandemics were associated with negative emotional states, anxiety about infection risk, disrupted routines, disruption of health care, financial and occupational concerns, and increased caregiving demands (Brooks et al., 2020; Rogers et al., 2020). Similar evidence is emerging from the COVID-19 pandemic related to greater rates of depression, anxiety, and stress among the general population (54% of 1,210 respondents to a survey in China; Wang et al., 2020) and, specifically, among mothers of infants and young children (Cameron et al., 2020). Among pregnant women with no preexisting mental disorders in Italy (N = 100), more than 50% indicated that the pandemic had a severe psychological effect on their well-being and reported greater levels of anxiety (Saccone et al., 2020). Anxiety was more severe for women in the first trimester of pregnancy (Saccone et al., 2020). Psychological distress among pregnant women appears to be driven by uncertainty and concern for older relatives, unborn children, other children, and their own health (Corbett et al., 2020). Given early evidence for psychological harm to pregnant women and the potential for lasting effects among new parents and infants, there is a need for nurses to address maternal mental health across all aspects of the perinatal care continuum.
- Because separation of mothers from infants can lead to negative growth and development and impaired bonding (Bartick, 2020; Bystrova et al., 2009; Stuebe, 2020), we recommend mothers and infants be kept together whenever safely possible. We recommend a trauma-informed approach to perinatal care for women and infants during the pandemic in consideration of the elevated potential for fear, anxiety, stress, grief, and other signs of psychological distress. A trauma-informed care approach involves recognizing and responding to these and other symptoms of trauma and actively seeking to avoid triggers and retraumatization while providing care (Substance Abuse and Mental Health Services Administration, 2014). Nurses can provide trauma-informed care during a pandemic by promoting women’s control and choice whenever possible, acknowledging the effects of COVID-19 on their births and early parenting experiences, and using a collaborative approach to ensure that their mental, physical, emotional, and social needs are met. This approach should be sustained beyond the pandemic because growing evidence suggests the value of and critical need for trauma-informed care for individuals who have experienced prior birth trauma, have histories of adverse childhood events, or have had negative life experiences that contribute to traumatic stress (Seng et al., 2009).”

June 26, 2020 – Journal of Gynecology Obstetrics and Human Reproduction[31] “Promotion of Maternal–Infant Mental Health and Trauma-Informed Care During the COVID-19 Pandemic”
- The aim of this study was to understand the consequences of pregnancy and fetal development, caused by infections by the SARS-CoV, MERS-CoV and SARS-CoV-2 viruses.
- For patients in general, the clinical characteristics resulting from contact with MERS-CoV, SARS-CoV, and SARS-CoV-2 can trigger an asymptomatic condition, mild symptoms such as a cold with or without fever. However, symptoms can progress to severe cases, corresponding to 25 % of patients infected with SARS-CoV-2, for acute respiratory distress, pneumonia, gastrointestinal problems, liver damage, septic shock, and multiple organ failure, which can lead to death. Especially in severe cases, SARS-CoV-2 may present multifocal nodular and ground-glass opacities surrounding the pulmonary lobes
- ..pregnant women show symptoms similar to non-pregnant women for Coronavirus
- The risk of viral pneumonia is significantly higher amongpregnant women compared to the general population, especially when there is no antiviral therapy
- There are no reports for vertical transmission, however, some newborns developed severe retardation in intrauterine growth and life-threatening gastrointestinal complications
- In the United States, in 2003, a study showed that two out of eight people with confirmed severe disease (SARS-CoV), were pregnant women.
- …there is no evidence that also SARS-CoV-2 can be transmitted transplacentally from the mother to the baby the treatment strategy for children with Covid-19 is based on the adult experience.
It is also important to highlight that the disease condition of mostchildrenis mild and, to date, few deaths in the pediatric age group have been reported
- CONCLUSION: Published obstetric cases reported the need for advanced life support for pregnant women infected with the coronavirus. Symptoms such as fever, chills, stiffness, myalgia, malaise, and cough, as well as laboratory data such as neutrophilia, lymphopenia, increased C-reactive protein, lactic dehydrogenase and aminotransferase were found at admission. This inflammatory status can promote conditions such as pre-eclampsia, premature birth, or growth restriction intra-uterine. In fact,the fever, high blood pressure, pre-eclampsia, pneumonia, acute respiratory distress, and multiple organ failure, have been reported in the postpartum period, especially in pregnant women infected byMERS-CoV, which seems to be the most dangerous virus fornewborns. (This is not the same virus as SARS-CoV-2).
- Middle East Respiratory Syndrome (MERS) is a viral respiratory illness that is new to humans. It was first reported in Saudi Arabia in 2012 and has since spread to several other countries, including the United States. Most people infected with MERS-CoV developed severe respiratory illness, including fever, cough, and shortness of breath. Many of them have died.[32]
- Different studies affirmed that some pathophysiological changes were observed in the placentas of CoV-positive mothers. However, the vertical transmission for SARS-CoV and MERS-CoV viruses has not been detected, and few cases showed that the pregnancy resulted in intrauterine fetal death, congenital malformation (due to prematurity) or newborn death after emergency cesarean section. We believe that the coronaviruses infection on pregnant [women] can promote multiple disorders, such as shortness of breath, fever, elevated blood pressure, preeclampsia, pneumonia, and multiple organ failure, which can affect the fetus’s health. In relation to the few studies on SARS-CoV-2, as it is a new strain, it is still too early to draw conclusions.

June 26, 2020: The U.S. CDC (Centers for Disease Control and Prevention) Morbidity and Mortality Weekly Report[33] released on June 26 analyzed data among pregnant women in the United States between January 22 and June 7, 2020. Findings mirrored a recent study in Sweden.[34]
In the U.S., pregnant women were more than 5 times more likely to be hospitalized and 1.5 times more likely to be admitted to the ICU. In Sweden, pregnant women were five times more likely to be admitted to the ICU, than non-pregnant women. Interestingly, symptoms like fever, aches, chills, headache and diarrhea occurred less in pregnant women, than their non-pregnant counterparts.
Risk of death was the same, however.
Specific details include: “Among women with COVID-19, approximately one third (31.5%) of pregnant women were reported to have been hospitalized compared with 5.8% of nonpregnant women. After adjusting for age, presence of underlying medical conditions, and race/ethnicity, pregnant women were significantly more likely to be admitted to the intensive care unit (ICU) confidence interval and receive mechanical ventilation…These findings suggest that among women of reproductive age with COVID-19, pregnant women are more likely to be hospitalized and at increased risk for ICU admission and receipt of mechanical ventilation compared with nonpregnant women, but their risk for death is similar…The percentages of pregnant women reporting fever, muscle aches, chills, headache, and diarrhea were lower than those reported among nonpregnant women, suggesting that signs and symptoms of COVID-19 might differ between pregnant and nonpregnant women…data needed to distinguish hospitalization for COVID-19 from hospital admission for pregnancy-related conditions were not available…Further, differences in hospitalization by pregnancy status might reflect a lower threshold for admitting pregnant patients…”[35]
- According to the CDC report, there were at least four limitations to the findings:
- Pregnancy status (whether or not any of the 326,335 people in the study were pregnant) was missing in the majority of women, which can lead to “overestimation or underestimation.”
- Additional time may be necessary to fully ascertain the significance of outcomes like ICU admission, ventilation and death. For example, will the numbers be higher after a few more months of pregnancy?Information on “whether or not the hospitalization was related to pregnancy conditions rather than for covid-19 illness was not available.” What if hospitalization is being caused by common pregnancy conditions instead of coronavirus?
- “Routine case surveillance does not capture pregnancy or birth outcomes; thus, it remains unclear whether SARS-CoV-2 infection during pregnancy is associated with adverse pregnancy outcomes, such as pregnancy loss or preterm birth.”
Is it safer for expecting women who want to avoid their babies from contracting Covid-19 to select C-section as their birth plan? Are isolation away from one’s newborn as well as avoidance of breastfeeding (use of formula) important in saving one’s newborn from the syndrome caused by SARS-CoV-2?
The BJOG, an International Journal of Obstetrics and Gynaecology wanted to find out if these early rumors were true, and published their findings on June 12, 2020. Researchers examined 49 studies which included more than 600 babies and women. Of the women who delivered via Cesarean, 5.3% confirmed COVID-19 infection, compared to 2.7% of the babies born vaginally. Authors stated, “Newborn infants can be infected in the first few hours of life, but as very few are severely affected it is likely that the benefits of contact with the mother and the ability to breast feed outweigh the potential benefits of separation.”[36]
A June 8, 2020, release in the Journal of American Medical Association (JAMA), wondered why coronavirus data from China found severe complications in so many pregnant women, and whether method of delivery could have been the cause. Researchers looked at 82 pregnancy cases of (SARS-CoV-2) in Spain between March 12 and April 6. Several of the women still had severe COVID-19 symptoms at delivery, but the majority presented with no or mild symptoms. About half birthed vaginally and the other half birthed via C-section. (Eight of the C-sections were doneso due to “Covid-19 symptoms, without other obstetrical indications.”) The report discussed these important take-away messages:
- Vaginal births with excellent outcomes: “Among patients with mild symptoms at presentation, all patients with a vaginal birth had excellent outcomes.”
- Cesarean births with severe outcomes and deterioration: “In contrast, 13.5% of women undergoing cesarean delivery had severe maternal outcomes and 21.6% had clinical deterioration.”
- Regardless of COVID-19, Cesarean births show higher risks of adverse outcomes: “Women undergoing cesarean delivery may have been at higher risk of adverse outcomes, but after adjusting for confounding factors, cesarean birth remained independently associated with an increased risk of clinical deterioration. The physiological stress induced by surgery is known to increase postpartum maternal complications. Cesarean delivery was also associated with an increased risk of NICU admission.”
On June 15, 2020, Evidence Based Birth shared the following in an email[37] of compiled research on COVID-19:
- “The data do not show an increase in the rate of infection with vaginal birth.”
- “The data do not show an increase in the rate of infection with breastfeeding.”
- “The data do not show an increase in the rate of infection with rooming in. Furthermore, newborn infection has been shown to occur despite isolation.”
- “In summary, newborn infection is uncommon and rarely causes symptoms…the rate of infection was not increased when the baby was born vaginally, breastfed/chestfed, or had contact with the infected birther.”
- “The majority of poor outcomes relate to increased preterm birth and high Cesarean rates”
- The “absence” of COVID-19 transmission directly from mother to baby is “reassuring.”
- Update on Testing Accuracy: “Even when timing is optimal, tests may miss about 1 in 5 infections.” (Tests are more accurate when taken about 8 days after exposure, or 3 days after symptoms start.)
- Update on Mask Wearing: “The researchers concluded that wearing face masks in public is the single most effective way to prevent SARS-CoV-2 transmission.”

May 22, 2020: The American Journal of Clinical Pathology examined the health of placentas in 16 women who tested positive for COVID-19, and who delivered between March 18 and May 5, 2020. Compared to control placentas of what is understood to be otherwise healthy, the women who had COVID-19 showed, “a pattern of placental injury reflecting abnormalities in oxygenation within the intervillous space associated with adverse perinatal outcomes.”[38]
As explained by Science Daily[39], interviewing co-author of the study, Dr. Emily Miller: “‘The placenta acts like a ventilator for the fetus, and if it gets damaged, there can be dire outcomes,’ Miller said. ‘In this very limited study, these findings provide some signs that the ventilator might not work as well for as long as we’d like it to if the mother tests positive for SARS-CoV2.’” According to the Science Daily report, “The placentas in these patients had two common abnormalities: insufficient blood flow from the mother to the fetus with abnormal blood vessels called maternal vascular malperfusion (MVM) and blood clots in the placenta, called intervillous thrombi.”
Regardless, the newborns were considered healthy: “Placentas get built with an enormous amount of redundancy. Even with only half of it working, babies are often completely fine. Still, while most babies will be fine, there’s a risk that some pregnancies could be compromised.”[40]
Some shortcomings of the study include:
- Researchers have not done similar studies to check the placentas of pregnant women who have suffered other “influenza-like illness.”[41]
- The possibility that the cause of the placental pathology may be, for example, the mental-emotional stress accompanying ‘testing positive’ for COVID-19 within the unknown atmosphere of terror of this initially completely foreign disease. Will pregnant women who have COVID-19 in future years, after it becomes “normal”, still have placental pathology? As researchers noted, “our study does not formally test causality or the direct relationship between SARS-CoV-2 infection and development of placental pathology.”[42]
A March 31, 2020, report in Exercise Immunology Review was called, “Regular exercise benefits immunity — even in isolation.”[43] As reported by Science Daily who interviewed authors Campbell and Turner, “Provided it is carried out in isolation — away from others — then regular, daily exercise will help better maintain the way the immune system works — not suppress it.” As one of the Five Foundations of human health, movement is a key component for the optimal function of humanity, and that is especially true in this new age of COVID-19.
A research paper from the Journal of Psychiatric Research, made available on May 25, 2020, identified that “Higher choline levels obtained through diet or supplements may protect fetal development and support infant early behavioral development even if the mother contracts a viral infection in early gestation when the brain is first being formed.”[44] Specifically, infants of mothers who had a moderately severe respiratory virus along with high choline levels had better attention and bonding with their parents, compared to infants whose mothers got sick but had low levels of choline. “Choline is a recently discovered nutrient. It was only acknowledged as a required nutrient by the Institute of Medicine in 1998. Although your body makes some, you need to get choline from your diet to avoid a deficiency.”[45] Choline is needed for things like: cell structure, cell messaging, fat transport and metabolism, DNA synthesis, and healthy nervous system. Pregnant women may need about 450mg daily (requirements increase during pregnancy). Sources of choline include:
- Beef & chicken liver
- Eggs
- Fresh cod, salmon
- Cauliflower, broccoli
This graphic, created by Science Direct, represents how choline’s role in immunity may beneficially affect infants whose mothers become infected by moderately severe respiratory virus infections.
How COVID-19 Deaths are Counted
“The challenge is knowing who died of COVID-19 versus who died with the virus that causes COVID-19.”
Scientific American,May 19, 2020
Dr. Jeremy Faust, Emergency Physician, Brigham and Women’s Hospital in Massachusetts, USA
The May, 2020, edition of Irish Medical Journal discussed Vitamin D requirements, COVID-19, and the fact that people are commonly indoors more (away from the sun and it’s Vitamin D contribution). “Vitamin D determines severity in COVID-19,”[47] reported Science Direct, discussing how the study found that the countries with the lowest rates of COVID infection and death were those that have the highest Vitamin D levels. Science Daily further explained, “Many recent studies confirm the pivotal role of vitamin D in viral infections…The correlation between low vitamin D levels and death from COVID-19 is statistically significant. The authors propose that, whereas optimising vitamin D levels will certainly benefit bone and muscle health, the data suggests that it is also likely to reduce serious COVID-19 complications.”[48]
Vitamin D recommendations for women in childbearing years is commonly around 600 IU.[49] But according to the American Pregnancy Association, “A recent study found women taking 4,000 IU of vitamin D daily had the greatest benefits in preventing preterm labor/births and infections.”[50]
Sources of Vitamin D include:
- Spend time outdoors & in sunlight
- Fatty fish and seafood: salmon, cod liver oil
- Mushrooms
- Egg yolks & beef liver & cheese (“small amounts”[51])
If you use a Vitamin D supplement, keep in mind that Vitamin D3 is preferred to D2 due to its effectiveness [52] and because this is the kind that is naturally made by the body[53].
[1]https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it
[2] https://www.cdc.gov/nchs/data/dvs/lcwk/lcwk3_hr_2016.pdf
[3] https://www.cdc.gov/nchs/data/dvs/lcwk/lcwk3_hr_2016.pdf
[4] https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_09-508.pdf
[5] https://www.cdc.gov/nchs/products/databriefs/db355.htm
[6] https://www.cdc.gov/nchs/products/databriefs/db355.htm
“In 2018, a total of 2,839,205 resident deaths were registered in the United States—25,702 more deaths than in 2017.” – CDC Report: “Mortality in the United States, 2018”
[7] https://www.cdc.gov/nchs/products/databriefs/db355.htm
[8] https://www.cdc.gov/nchs/nvss/vsrr/provisional-tables.htm
[9]https://www.cdc.gov/nchs/products/databriefs/db395.htm
“In 2019, a total of 2,854,838 resident deaths were registered in the United States—15,633 more deaths than in 2018.” – CDC Report: “Mortality in the United States, 2019”
[10] https://www.cdc.gov/nchs/nvss/vsrr/mortality-dashboard.htm
[11] https://www.cdc.gov/nchs/fastats/deaths.htm
[12] https://www.cdc.gov/nchs/fastats/deaths.htm
[13] https://www.cbs19.tv/article/news/health/coronavirus/verify-comparing-the-number-of-total-deaths-in-the-united-states-across-years/501-2aacbd08-466a-4d17-8452-e059df9aa6f3
[14] According to Evidence Based Birth, email sent Dec. 8, 2020, titled, “Research Update on COVID-19 and Pregnancy: Special Edition on Vaccines”
[15] https://pubmed.ncbi.nlm.nih.gov/12667025/
[16] https://www.bloomberg.com/news/articles/2020-11-09/pfizer-vaccine-s-funding-came-from-berlin-not-washington
[17] https://www.cdc.gov/vaccines/covid-19/hcp/mrna-vaccine-basics.html
[18] https://www.news-medical.net/health/What-is-an-Inactivated-Vaccine.aspx
[19] https://www.niaid.nih.gov/research/vaccine-types
[20] https://www.news-medical.net/health/What-is-an-Inactivated-Vaccine.aspx
[21] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6668849/
[22] https://www.the-scientist.com/news-opinion/vector-based-vaccines-come-to-the-fore-in-the-covid-19-pandemic-67915
[23] https://www.the-scientist.com/news-opinion/vector-based-vaccines-come-to-the-fore-in-the-covid-19-pandemic-67915
[24] https://www.news-medical.net/health/What-are-Spike-Proteins.aspx
[25] https://vaccine-safety-training.org/subunit-vaccines.html
[26] https://www.cdc.gov/vaccines/vac-gen/additives.htm
[27] https://www.bloomberg.com/news/articles/2020-11-09/pfizer-vaccine-s-funding-came-from-berlin-not-washington
[28] https://www.cnbc.com/2020/05/21/coronavirus-us-gives-astrazenena-1-billion-for-oxford-vaccine.html
[29]https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1411/5908705
[30] https://www.jognn.org/article/S0884-2175(20)30115-5/fulltext
[31]https://www.sciencedirect.com/science/article/pii/S2468784720301902?via%3Dihub
[32] https://www.cdc.gov/coronavirus/mers/index.html
[33]https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6925a1-H.pdf
[34] “These findings are similar to those from a recent study in Sweden, which found that pregnant women with COVID-19 were five times more likely to be admitted to the ICU and four times more like to receive mechanical ventilation than were nonpregnant women.” https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6925a1-H.pdf
[35]https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6925a1-H.pdf
[36]https://obgyn.onlinelibrary.wiley.com/doi/pdf/10.1111/1471-0528.16362
[37] Covid-19 Research Update summary (Email sent Jun 15, 2020, 10:58 AM;Evidence Based Birth)
[38]https://academic.oup.com/ajcp/article/154/1/23/5842018
[39]https://www.sciencedaily.com/releases/2020/05/200522113714.htm
[40]https://www.sciencedaily.com/releases/2020/05/200522113714.htm
[41]https://academic.oup.com/ajcp/article/154/1/23/5842018
[42]https://academic.oup.com/ajcp/article/154/1/23/5842018
[43]https://www.sciencedaily.com/releases/2020/03/200331162314.htm
[44]https://doi.org/10.1016/j.jpsychires.2020.05.019
[45]https://www.hehttps://www.sciencedaily.com/releases/2020/03/200331162314.htmalthline.com/nutrition/what-is-choline#what-it-is
[46] Image:https://www.sciencedirect.com/science/article/pii/S0022395620304544?via%3Dihub
[47]https://www.sciencedaily.com/releases/2020/05/200512134426.htm
[48]https://www.sciencedaily.com/releases/2020/05/200512134426.htm
[49]https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
[50]https://americanpregnancy.org/pregnancy-health/vitamin-d-and-pregnancy/
[51]https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/#:~:text=Food,%2C%20cheese%2C%20and%20egg%20yolks.
[52]https://www.healthline.com/nutrition/vitamin-d2-vs-d3#:~:text=Most%20studies%20show%20that%20vitamin,raising%20calcifediol%20levels%20(%209%20).
[53]https://www.webmd.com/osteoporosis/features/the-truth-about-vitamin-d-what-kind-of-vitamin-d-is-best
