While the thought of breech birth can feel ominous, expectant mothers can navigate this potential obstacle confidently when equipped with the right information and support. This article covers everything you want to know.

What is a Breech Baby?
In the vast majority of pregnancies, babies will naturally position themselves head down, chin tucked to chest, facing their mother’s back. And this is the position known for generally allowing the smoothest labor & delivery[1]. Comparatively, baby’s head down but facing forward, known as “sunny side up,” is associated with a longer and less comfortable delivery experience.
Breech birth, however, has such a stigma associated with it, that the option for a vaginal delivery is not even available in some countries.[2]

Breech presentation is when a baby is positioned to deliver feet or buttocks first. It occurs in 3-4% of full-term pregnancies. There are few kinds of breech presentations:
- Frank Breech – Fetus’s buttocks are aimed toward the birth canal with straight legs, and feet near the head.
- Complete / Full Breech – Fetus’s buttocks are pointed down, but knees folded and feet near buttocks.
- Incomplete / Footling Breech – When one or both of the fetus’s feet are pointed toward the birth canal, positioned to deliver first. This could be single or double, depending how many feet are positioned to deliver first.
- Kneeling Breech – Knees positioned to deliver first.
There is also the possibility of the baby lying sideways, horizontally (transverse).
A key point in breech is when the breech is present. Check where you are in your pregnancy, compared to the natural progression if you do nothing:
| Weeks into pregnancy | Percentage of breech babies [3] |
| < 28 weeks | 25% |
| 32 weeks | 7% |
| “Full term” (Between 39 weeks, 0 days and 40 weeks, 6 days) | 3-4% |
| Beyond full term | 3% |
| Once at full term, the likelihood of a breech position naturally correcting to a head-down position is rare, happening in fewer than 10% of first-time pregnancies. [4] | |
The first thing to understand is that your baby is likely to naturally turn on his or her own, if you do nothing more than let nature take its course. However, still presenting with a breech at full term is when mothers and medical professionals have to make decisions about their birth options. Let’s dive into understanding the cultural climate, the implications and the evidence-backed options available for a healthy delivery journey.

Why do we expect breech babies to be born via c-section?
Before 1940, breech presentations were associated with an infant death rate of approximately 5%, but c-sections were so dangerous to the mother that they were not used routinely.[5] This meant that birth attendants had plenty of practice in attempting vaginal breech deliveries, as would have been true throughout ancient times as well. There is a skill that comes from experience of this practice.
Then a significant turning point occurred in the year 2000 when the “Term Breech Trial” (TBT) led to a sharp increase in the rate of c-sections for breech presentations. Using 121 centers, 26 countries, and 2088 women with breech presentation, this landmark study found that likelihood of infant death was significantly lower for the planned c-section breech group than for the planned vaginal breech birth group. [6] Although significant criticism for this study would emerge [7] [8], even calling for a recommendation for the trial to be withdrawn [9], c-sections became the new standard for breech babies.
What do I do if I’m breech? 3-step overview
Breech birth is significant, affecting about 1 in 25 pregnancies. Although this article will explore all of this in more detail, the overview is:
- Consider doing some of the more natural and non-invasive techniques for turning a baby head-down. Do these earlier, in the 30-37th weeks of pregnancy.
- If still breech at 37 weeks, consider discussing an External Cephalic Version (ECV) with a birth professional.
- If still breech at 39 weeks and beneficial predictors of vaginal birth are present, vaginal birth is an option, but if predictors are not present, opt for elective c-section. (In many cases, it is at this time that you would be “required” to opt for the c-section because staff is not accustomed to delivering breech vaginally. The other option would be to switch your birth team in the final weeks.)
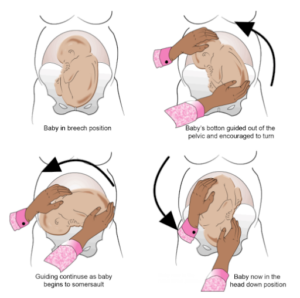
What is ECV?
External Cephalic Version (ECV or EV) is when a trained healthcare professional applies firm pressure to your belly, attempting to physically turn your baby’s head down, thereby “solving” the breech. Essentially:
- External means that pressure will be applied to your belly
- Cephalic refers to “cephalic presentation,” the ideal labor-ready position when the baby’s head is down, and facing the mother’s back.
- Version is the act of turning or rotating, in this case specifically referring to this hands-on procedure.
ECV gives the chance for the optimal vaginal birth position. This, in turn, can be the difference needed for medical providers to feel certain that a vaginal birth can be permitted, rather than requiring a c-section. ECV can be rather uncomfortable, even to the point of deciding not to continue, and there are risks of fetal distress which requires conscious monitoring.
The objective of ECV is to achieve cephalic presentation. The evidence for attempting ECV is rather robust and generally positive at this point.
- A 2012 Obstetrics and Gynaecology Review [10] found that ECV should be offered to all breech pregnancies who do not have contraindications. It also suggested an individualized approach for unsuccessful ECV’s, which includes creating awareness of vaginal delivery of certain breech presentations being a reasonable option, and including counsel on risks associated with c-sections.
- A 2023 Labour and Delivery [11] study suggested using ECV for suitable patients, followed by c-section at 39 weeks if they are not good candidates for ECV. Furthermore, authors suggested that if the patient goes into labor, a vaginal breech can be considered “if the predictors of vaginal birth are present.” Finally, they recommended including more practice in labor rooms, “to improve the expertise for the health care professionals in conducting vaginal breech deliveries.”
So, there is good evidence for ECV being a useful option.
What is Cephalic Presentation?
Cephalic Presentation is considered the least complicated and most ideal position for the baby to be for vaginal delivery: head down, chin tucked to chest, facing their mother’s back.
And of course the big question is, “How many different ways are there to encourage my baby to move into that optimal cephalic position?”
There are a number of methods available to try! Some of the methods have research studies showing reliable results, while some of the methods don’t have a lot of research-backing, but could still be options to consider. We review them below.
Potential Methods for Encouraging Head-Down Babies
There are a variety of methods for turning a baby from breech to head down. Some require manual manipulation (with or without medicines). Others use acupressure points. And others seem to involve relaxation, positioning of the pregnant body, homeopathy and/or postural mechanics.
OVERVIEW of methods for turning breech babies head-down
Of the various research-proven methods for turning a breech baby, one of the first stops is ECV which was mentioned above. This can be done with or without medications. Tocolysis refers to using medications intended to delay fetal delivery in order to provide a window of time for support treatments to be implemented. [12] Essentially, tocolytic medications are designed to delay or weaken uterine contractions, commonly used for delaying premature birth. See here for a thorough overview of tocolysis.
→Based upon the size and results of various studies, it appears that medically relaxing the uterus (ECV), medically numbing the tummy (ECV), and moxibustion can be considered the leading methods that have been research-validated enough to provide certainty. This doesn’t mean they will work every time, but it does mean that they do appear to consistently work better than doing nothing. Note that medically relaxing & numbing would be done in conjunction with ECV, whereas moxibustion may occur spontaneously, without needing the external manipulation.
→Hypnosis prior to ECV, lying inverted, Webster chiropractic technique, pulsatilla, and Spinning Babies show weaker evidence, but are reasonable possibilities for being helpful. Note also that, except for hypnosis, these techniques would generally be considered to occur spontaneously, without the manual manipulation of ECV.
→Finally, we’ll briefly review two methods for which no evidence has been found: amnioinfusion & fetal acoustic stimulation.
SPECIFIC STUDIES to understand where the evidence points for encouraging head-down babies.
Medically Relax the Uterus (ECV): A 2015 systematic review considered 28 studies and 2786 women. It found parenteral beta stimulants to be effective in successful ECV and thereby reducing the c-section rate, although data on adverse effects were insufficient. [13] Authors of this huge review wrote of the “possible benefits of tocolysis in reducing the force required for successful version.”
- This same 2015 systematic review found insufficient data for the use of calcium channel blockers, nitric acid donors, fetal acoustic stimulation, amnioinfusion, and hypnosis in ECV. [Note that nitric oxide donors, and also nitroglycerine (2014 finding[14]), should be discouraged due to “sufficiently negative” outcomes.]
- A 2023 study of 207 women found terbutaline injection (another medication that can relax the uterus) associated with successful ECV, as was having more amniotic fluid and an infant with a smaller head size in relation to its femur length. [15]
- A previous 2004 systematic review had supported the confirmation that tocolysis helps the success rate of ECV as well. [16]
Medically numb the tummy (ECV): A 2016 study in AJOG, of 934 women, found that using another medication— this time one intended to numb the tummy—“significantly increases the success rate of [ECV] among women with malpresentation at term or late preterm, which then significantly increases the incidence of vaginal delivery.” [17] In this case, the medicine was neuraxial analgesia, which is injected into the spinal fluid. [18]
- ECV without Anesthesia: A 2021 study in the Journal of International Medical Research, used only 40 cases, but concluded that ECV after 37 weeks “without anesthesia is an effective and relatively safe alternative” that can reduce c-section rate. [19] (Terbutaline was still used to relax the uterus.)

Consider Moxibustion: A 2023 systematic review on moxibustion [20], which considered 13 studies and 2181 women, found “moderate‐certainty evidence that moxibustion plus usual care probably reduces the chance of non‐cephalic presentation at birth.” In other words, burning a type of Chinese medicine herb close to the skin at a certain acupuncture point (BL67) probably works for bringing babies into head-down position.
- A 2019 study [21] found that adding acupuncture (needle stimulations) in addition to moxibustion may also be effective for inducing head-down babies.
Moxibustion kits, which can be purchased online, or from Chinese Medicine doctors, should be started before week 37. [22] One curiosity is that even though babies do often turn head down, the overall rate of c-section in these studies ended up remaining similar to those without moxibustion.

Consider Hypnosis & Relaxation: A 2012 study in the American Journal of Hypnosis [23]compared 78 women with hypnosis intervention prior to ECV versus 122 who received only standard medical care. The conclusion was that relaxation with the help of hypnosis “was successful at increasing the likelihood of a successful ECV procedure” (41.6% success for hypnosis vs 27.3% without hypnosis).
(Remember that the 2015 Systematic Review of ECV found “insufficient data” for hypnosis.)
Consider Lying Inverted: In 2002, 46 mothers determined to have a breech baby at 30 weeks were instructed to lie on their back with legs inverted at a 45-degree angle. At 37-weeks, anyone still presenting breech was sent for ECV. Comparing the usual 3-4% breech stats, they found “significantly fewer breech presentations following this kind of “postural management.” [24]
The Webster Chiropractic technique was identified initially due to observations by pregnant women and their chiropractors that this particular sacral adjustment corrected babies to head-down position. One 2002 survey of 112 chiropractors found that 92% reported “resolution of the breech presentation.” [25]
Way back in 1871, thirty pellets of pulsatilla were given to a woman with a transverse baby. She reported that her baby turned within 2 hours of taking this homeopathic or herbal remedy. [26] Pulsatilla comes from the pasqueflower plant, and is thought to calm muscle spasms and help with reproductive issues, among other things. A 2021 study found pulsatilla extract to inhibit cancer cells [27], while a 2022 study found homeopathic pulsatilla to cure one “young female” with PCOD (polycystic ovary disease). [28]
Some of you may be familiar with the Spinning Babies non-pharmacological technique that “assists women with position changes throughout labor.” [29] As described on their website, this technique doesn’t want you too tight nor too loose, the first of their three principles, they call balance. The other two principles are alignment in gravity, and moving throughout the day. A 2023 study in the College of Nursing [30] looked at the medical records of 400 women who used the Spinning Babies method, comparing them to 858 women who did not use the method. There were two main findings:
- Spinning Babies method yielded 84% to deliver vaginally compared to 77% among conventional laborers.
- Conventional laboring women experienced a shorter duration of labor than those who did Spinning Babies.
So, Spinning Babies appears to offer slightly better chances of avoiding c-section, but at the cost of spending longer time in labor.
Amnioinfusion places extra fluid inside the uterus, using an intrauterine pressure catheter. Could this help to create enough space within the uterus to allow the baby to be moved head-down via ECV? A 2018 study in the Journal of Maternal-Fetal & Neonatal Medicine studied 119 women and found that amnioinfusion prior to ECV did not produce cephalic presentation more than those who did not receive the fluid-injection. [31]
Fetal acoustic stimulation involves using sound to stimulate fetal activity, with the hope that this increased activity might lead to the fetus turning spontaneously. A device that produces sound is placed on the mother’s abdomen near where the fetus’s head is located. The idea is that the sound will stimulate the fetus, causing it to move and potentially turn to a head-down position. While there is anecdotal evidence that fetal acoustic stimulation can encourage fetal movement, various scientific studies have concluded there is insufficient evidence.
What should I be careful to avoid?
Side effects of medication: First, one should be careful with the use of pharmaceutical medications for ECV in general. As noted in the 2015 systematic review, the “data on adverse effects” of parenteral beta stimulants were “insufficient.” [32] In other words, ECV works to help babies go head down, but we don’t know much about any side effects to the medications used.
Side effects of manual manipulation: Next, the act of manually rotating via ECV can be harsh on you and your baby. “Complications such as vaginal bleeding, placental abruption, preterm rupture of membranes and fetal distress” are rare, but may occur. [33] It sucks to put your baby through stress that may cause his or her short-term heart rate (HR) abnormalities. HR abnormalities during and after ECV tend to be more frequent for smaller birth weight babies and during longer ECV procedures.
Which breech position is easiest to deliver?
When attempting a vaginal breech delivery, frank breech presentation appears to be the easiest to attempt, with complete (flexed) and incomplete (footling) being doable so long as the presenting part is firmly positioned against the cervix. [34]
How necessary is it to turn my baby head-down?
On the natural human front, it is quite possible to deliver a breech baby, especially if you fit certain criteria and can find a skilled, supportive professional. This is a decision that will depend upon each mother’s personal circumstances.
The criteria include things like [35]:
- Not having a very low birth weight baby
- Not having congenital malformations
- Not having premature labor
- (Possibly others; see more discussion below)
In fact, a 2007 study of 165 breech and 165 cephalic vaginal deliveries showed that the perinatal deaths that do occur are “not related to the mode of delivery” with no “statistically significant differences in mortality between the vaginally delivered group and the Caesarean section group” of breech babies. [36] This study called breech deaths “unavoidable” which means that vaginal delivery of the breech was not the cause of death.
This information is perhaps partly accounted for when one is made aware that the likelihood of having a baby that continues to present in the breech position also correlates with older maternal age, first time birth, fluid build-up in the infant brain, established maternal diabetes, and smoking during pregnancy, “suggesting that there may be several different biologic mechanisms leading to breech presentation.” [37]
| Weeks into pregnancy | Likelihood of Breech arising from: |
| 24-27 |
|
| 28-31 |
|
| 32-36 |
|
Table: This chart rises from a 2019 study showing that “Breech presentation in preterm labor is associated with obstetric risk factors.” [38]
Sorting through criteria like these, a 2018 study in BMC Pregnancy and Childbirth, that followed a single obstetrician practice for 6 years, concluded that “Out-of-hospital vaginal breech birth under specific protocol guidelines and with a skilled provider may be a reasonable choice for women wishing to avoid a cesarean section—especially when there is no option of a hospital breech birth.” [39] It has also been found in an official panel of midwives and obstetricians, that the ideal model of care for breech at term is midwifery-led continuity of care with supportive obstetric consultant input. [40]
If you or your client determines that you match the criteria for delivering a vaginal breech, you must then find a qualified birth professional who can help you.
Believe it or not, there are some who are relatively accustomed to, and even skilled at, delivering breech babies. This lost art is being rebirthed in some settings. Remember, since 2000, the shift in hospitals has been toward c-section, making it less likely to find skilled professionals in that specific setting. It is also the case that regional laws can make it challenging to find someone who can deliver breech legally. One organization, called Breech Without Borders offers a directory to get you started in finding a birth professional that can help you.
Wishing you clarity and peace of mind,
james
If you would like fun guidance during your own pregnancy, postpartum, or as a fitness professional, please check out these Fit For Birth offerings:
- Pregnancy & Postpartum:
- Pregnancy & Pre-conception: Online Pregnancy Program
- Fitness & Wellness Professionals:
James Goodlatte is a Father, Holistic Health Coach, Corrective Exercise Practitioner, Speaker, Author, Professional Educator, and the founder of Fit For Birth. Since 2008, when he found out he would be a father, his passion for holistic wellness shifted to children and families. Today, he is a driving force in providing Continuing Education Credits for the pre and postnatal world, with Fit For Birth professionals in 52 countries. James is also the program director for Fit For Birth pre & postnatal personal training worldwide, and is a contributing member of the First 1000 Days Initiative at the Global Wellness Institute.
REFERENCES
[1] Your Guide to Fetal Positions before Childbirth. Penn Medicine Health Hub. Retrieved 3/8/24 from https://www.lancastergeneralhealth.org/health-hub-home/motherhood/your-pregnancy/your-guide-to-fetal-positions-before-childbirth
[2] 2020. Tsakiridis, et al. Management of Breech Presentation: A Comparison of Four National Evidence-Based Guidelines. Perinatology. Retrieved 3/7/24 from https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-0039-1692391
[3] 2022. Gray & Shanahan. Breech Presentation. StatPearls [Internet]. Retrieved 3/8/24 from https://www.ncbi.nlm.nih.gov/books/NBK448063
[4] 2020. Tsakiridis, et al. Management of Breech Presentation: A Comparison of Four National Evidence-Based Guidelines. Perinatology. Retrieved 3/7/24 from https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-0039-1692391
[5] 2020. Tsakiridis, et al. Management of Breech Presentation: A Comparison of Four National Evidence-Based Guidelines. Perinatology. Retrieved 3/7/24 from https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-0039-1692391
[6] 2000. Hannah, et al. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. The Lancet. Retrieved 3/8/24 from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(00)02840-3/abstract
[7] 2004. Iams, Jay. The Term Breech Trial. AJOG. Retrieved 3/8/24 from https://www.ajog.org/article/S0002-9378(04)00905-6/fulltext#back-bib1
[8] 2007. Bewley & Shennan. Peer review and the term breech trial. The Lancet. Retrieved 3/8/24 from https://www.thelancet.com/article/S0140-6736(07)60447-4/fulltext
[9] 2005. Glezerman, Marek. Five years to the term breech trial: The rise and fall of a randomized controlled trial. AJOG. Retrieved 3/8/24 from https://www.ajog.org/article/S0002-9378%2805%2901362-1/abstract
[10] 2012. Cluver & Hofmeyr. Breech presentation : the controversy continues : review. Obstetrics and Gynaecology Forum. Retrieved 3/7/24 from https://journals.co.za/doi/abs/10.10520/EJC73404
[11] 2023: Lalwani, et al. Breech Presentation. Labour and Delivery. Retrieved 3/6/24 from https://link.springer.com/chapter/10.1007/978-981-19-6145-8_5
[12] 2023. Mayer & Apodaca-Ramos. Tocolysis. StatPearls [Internet]. Retrieved 3/11/24 from https://www.ncbi.nlm.nih.gov/books/NBK562212/
[13] 2015. Cluver, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Library. Retrieved 3/3/24 from https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000184.pub4/full
[14] 2014: Cluver, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. Retrieved 3/7/24 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4171393/
[15] 2023. Duan, et al. Preoperative predictors of successful External Cephalic Version with breech presentation at term: a single centre experience. Research Square [pre-print]. Retrieved 3/6/24 from https://www.researchsquare.com/article/rs-3233793/v1
[16] 2004. Hofmeyer & Gyte. Interventions to help external cephalic version for breech presentation at term. Cochrane Database of Systematic Reviews. Retrieved 3/7/24 from https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000184.pub2/abstract
[17] 2016. Magro-Malosso, et al. Neuraxial analgesia to increase the success rate of external cephalic version: a systematic review and meta-analysis of randomized controlled trials. American Journal of Obstetrics and Gynecology. Retrieved 3/7/24 from https://www.sciencedirect.com/science/article/abs/pii/S000293781630134X
[18] [n.d.] Society for Obstetric Anethesia and Perinatology. Retrieved 3/11/24 from https://soap.memberclicks.net/assets/2023EducationMaterials/06E%20ECV%20Patient%20Education.pdf
[19] 2021. Zhi & Xi. Clinical analysis of 40 cases of external cephalic version without anesthesia. Journal of International Medical Research. Retrieved 3/12/24 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7812407
[20] 2023. Coyle, et al. Cephalic version by moxibustion for breech presentation. Cochrane Database of Systematic Reviews. Retrieved 3/7/24 from https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003928.pub4/abstract
[21] 2019. Brici, et al. Turning Foetal Breech Presentation at 32-35 Weeks of Gestational Age by Acupuncture and Moxibustion. Hindawi. Retrieved 3/7/24 from https://www.hindawi.com/journals/ecam/2019/8950924/
[22] 2023. Coyle, Smith, Peat. Moxibustion for turning a baby in breech position. Retrieved 3/8/24 from https://www.cochrane.org/CD003928/PREG_moxibustion-turning-baby-breech-position
[23] 2012. Reinhard, et al. Clinical Hypnosis Before External Cephalic Version. American Journal of Clinical Hypnosis. Retrieved 3/7/24 from https://www.tandfonline.com/doi/abs/10.1080/00029157.2012.665399
[24] 2002. Mattice Dancer, Michell. Effectiveness of a Postural Technique to Convert a Breech to a Cephalic Presentation. Thesis presentation to the Graduate School of The Ohio State University. Retrieved 3/8/24 from https://www.proquest.com/openview/6b9c440cf90dcf645722136d7a1ed44c/1?pq-origsite=gscholar&cbl=18750&diss=y
[25] 2002. Pistolese, Richard. The Webster Technique: A chiropractic technique with obstetric implications. Journal of Manipulative and Physiological Therapeutics. Retrieved 3/8/24 from https://www.sciencedirect.com/science/article/abs/pii/S0161475402000155
[26] 1871. Burt, W.H. Medical Investigator. Pulsatilla in Mal-presentation. Retrieved 3/8/24 from https://www.proquest.com/openview/55dc57b2618a98c20077408992bb1609/1?pq-origsite=gscholar&cbl=105827
[27] 2021. Łaska, et al. Extracts from Pulsatilla patens target cancer-related signaling pathways in HeLa cells. Scientific Reports. Retrieved 3/8/24 from https://www.nature.com/articles/s41598-021-90136-3
[28] 2022. Nadar & Athar. Pulsatilla in PCOD an Evidence Based Study. Journal of Medical and Pharmaceutical Innovation. Retrieved 3/8/24 from https://jmedpharm.com/index.php/home/article/view/173
[29] 2023, August. Sears, Darlene. The Impact of the Spinning Babies Method on Labor Duration and Delivery Outcome. Walden University Doctoral Dissertation. College of Nursing. ProQuest. Retrieved 3/8/24 from https://www.proquest.com/openview/b68a010f7dc0eb47477bb804668e0fa8/1?pq-origsite=gscholar&cbl=18750&diss=y
[30] 2023, August. Sears, Darlene. The Impact of the Spinning Babies Method on Labor Duration and Delivery Outcome. Walden University Doctoral Dissertation. College of Nursing. ProQuest. Retrieved 3/8/24 from https://www.proquest.com/openview/b68a010f7dc0eb47477bb804668e0fa8/1?pq-origsite=gscholar&cbl=18750&diss=y
[31] 2018. Diguisto, et al. Amnioinfusion for women with a singleton breech presentation and a previous failed external cephalic version: a randomized controlled trial. Journal of Maternal-Fetal & Neonatal Medicine. Retrieved 3/15/24 from https://pubmed.ncbi.nlm.nih.gov/28279119/
[32] 2015. Cluver, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Library. Retrieved 3/3/24 from https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000184.pub4/full
[33] 2017. Kuppens, et al. Fetal heart rate abnormalities during and after external cephalic version: Which fetuses are at risk and how are they delivered? BMC Pregnancy Childbirth. Retrieved 3/12/24 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5646157/
[34] 2022. Fischer, Richard, MD. Breech Presentation. Medscape. Retrieved 3/15/24 from https://emedicine.medscape.com/article/262159-overview?form=fpf#a2
[35] 2005. Ismail, et al. Comparison of vaginal and cesarean section delivery for fetuses in breech presentation. Journal of Perinatal Medicine. Retrieved 3/8/24 from https://www.degruyter.com/document/doi/10.1515/JPM.1999.047/html
[36] 2007. Noraihan Mohd. Nordin. An Audit of Singleton Breech Deliveries in a Hospital with a High Rate of Vaginal Delivery. Malays J Med Sci. Retrieved 3/8/24 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3351215/
[37] 1996. Rayl, et al. A population-based case-control study of risk factors for breech presentation. American Journal of obstetrics and gynecology. Retrieved 3/8/24 from https://www.sciencedirect.com/science/article/abs/pii/S000293789670368X
[38] 2019. Toijonen, et al. A comparison of risk factors for breech presentation in preterm and term labor: a nationwide, population-based case–control study. Maternal-Fetal Medicine. Retrieved 3/8/24 from https://link.springer.com/article/10.1007/s00404-019-05385-5
[39] 2018. Fischbein & Freeze. Breech birth at home: outcomes of 60 breech and 109 cephalic planned home and birth center births. BMC Pregnancy and Childbirth. Retrieved 3/8/24 from https://link.springer.com/article/10.1186/s12884-018-2033-5
[40] 2024: Morris, et al. Consensus-based recommendations for the care of women with a breech presenting fetus. Midwifery. Retrieved 3/3/24 from https://www.sciencedirect.com/science/article/pii/S0266613824000020
