This article is designed to guide you step-by-step to never having migraines again. Because of the elusive and individual nature of migraines, we need to start by teaching you a bit about how all the various triggers actually manifest inside your body. Migraines are chemical stressors being mismanaged within and around the cells. And that’s great news, because you have a tremendous amount of ability to adjust your internal chemistry. This article will show you how!
In addition, pregnancy causes the kind of internal chemical changes that can either reduce or increase the severity of migraines. Let’s make sure you’re doing everything you can to stop them once they’ve begun, as well as to prevent them from starting up again in the future.

What is a Migraine?
Migraines are a type of headache characterized by intense, throbbing pain that typically affects one side of the head. If you’re visiting this page in search of answers, you probably already knew that. The pain can be so debilitating that it is often accompanied by other symptoms such as nausea, vomiting, and extreme sensitivity to light and sound.
Migraine is the third most common disease worldwide, the most common neurological disorder, and one of the most common causes of chronic pain.[1] It is also one of the most common complaints in pregnancy.[2]
Migraines are associated with nerves & vessels in your brain
Migraines are currently understood to be caused by activation of the trigeminovascular system (TGVS).[3] The TGVS is a neural system connecting the brain to the blood vessels.[4] It includes both nerves and blood vessels leading into the brain. Within this system is the trigeminal nerve, which is one of the main nerves of the face. The trigeminal nerve is the largest nerve in your head. It provides sensory information, including pain signals between your head and brain, as well as to the blood vessels surrounding the brain.[5]
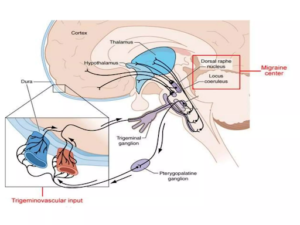
In addition, problems in nerve cell physiology, molecules released by the nerve cells, and nerve inflammation have become increasingly evident as causes of migraine.[8] All three of these components – physiology, molecules, and inflammation – refer to the natural chemical reactions that happen in the migraine-affected areas of your brain.
The usual culprits blamed for migraines
- Genetic predisposition
- External Environmental triggers
- Internal Neurochemical imbalances
Let’s do a brief overview of the implications of each, so that you can understand the deeper underlying causes beneath these “culprits.” Understanding the chemical nature of your migraines may be the most important factor in your ability to feel capable in making the lifestyle changes necessary to improve the function of your internal chemistry.
Genetic Predisposition
Genetic predisposition means that your parents gave you certain genes. In the case of migraines, you may have received genes that have a tendency to manifest migraines. While this may be true, it does not mean you are doomed to have migraines. Since the discovery of epigenetics, we now know that the most important factor is whether or not you turn those genes on or off, via the moment-by-moment lifestyle choices you make (more on that later).

For example, if two obese parents pass genes that increase the likelihood of obesity down to their child, that child is indeed statistically more likely to be obese. However, lifestyle choices such as exercise, nutrition, sleep, breathing, and stress management can significantly influence how these genes express themselves. Through these choices, the child can potentially mitigate some of the genetic risks. This can help reduce the likelihood of obesity by altering gene expression and promoting healthier physiological outcomes.
The same principle applies to parents who may have passed genes that increase the likelihood of migraines down their children. If the triggers for chemical inflammation are not chosen, it is much less likely that migraine-causing inflammation will appear in your brain, for example.
Visit one of these two epigenetic explanations if you want to understand how epigenetics changes the chemistry within and around your cells:
- What you need to know about epigenetics if you’re pregnant.
- 5 Steps of epigenetics of exercise: for fitness professionals.
External Environmental Triggers
Environmental triggers play a significant role in causing migraine attacks for many. These triggers can include things like[9]:
- Bright or flickering lights
- Loud noises
- Weather changes, such as shifts in barometric pressure
- Extreme temperatures, or high humidity
- Other pains, like tooth or neck pain
- Physical overexertion
- Strong smells like perfume or smoke
- Exposure to certain chemicals and pollutants in the environment
- Foods containing MSG & artificial sweeteners[10], or nitrates[11]
- Drinks like alcohol (especially red wine) and caffeine
Every external environmental stimulus must be “handled” by your internal stress-management systems, including the TGVS system. On a very basic level, the body only has two options: “fight or flight” or “rest & digest.” Both induce a very specific set of hormonal and chemical changes in the body. These self-induced chemical changes are specifically created to either (a) prepare internal chemicals for the “stress” of whatever event is underway (ie. noise, lights, temperature, pain, etc) or (b) counteract foreign chemical changes that are invading your system (ie. perfume, smoke, pollutants, artificial foods, etc).
If an external environmental trigger is noticeable enough that it must be “dealt with”, it means that your internal “fight or flight” response has been engaged, along with a whole slew of chemical and mechanical pressures into the brain.
→This is a form of stress management. If it is done “well” there is a chance that a migraine may not arise at all.
Theoretically, a healthy body should be able to handle these chemical and mechanical pressure shifts without suffering extreme pain of a migraine. But as more and more external environmental triggers add up, it becomes more difficult for that person’s internal biochemistry to react capably.
Stress & Pollutants must be managed for migraine relief
The above-list of environmental triggers for migraine can broadly be classified as either stress-related or pollutant-related. But both of these classifications ultimately boil down to whether or not your internal body chemistry can return to balance before a migraine is initiated.
Stress-related Chemical Disruptions: Dealing with stimuli such as bright/flickering lights, loud noises, weather/temperature changes, overexertion or pre-existing pains must constantly be managed, by every one. This kind of stress management is handled chemically, internally by the cells. Unfortunately, these stressors are enough to cause some people’s TGVS system to be unable to maintain, or quickly return to balance. This means it can be very challenging to achieve homeostasis, the term used to describe the process by which people maintain a stable internal environment, despite changes in their external environment.
Pollutant-related Chemical Disruptions: On the other hand, environmental triggers can also simply originate as direct chemical disruptions. If a migraine is triggered by perfumes, smoke, food chemicals, alcohol, or caffeine, etc, it is a sign that the internal chemical management pathways (detoxification pathways) may be overloaded by the chemicals that are entering from the outside. If overloaded, the TGVS would once-again have a really difficult time returning to homeostasis.

Neurochemical imbalances
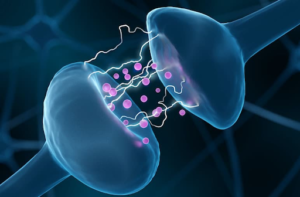
External environmental chemicals can trigger migraines, and so can internal neurochemical imbalances, even if external triggers are not present. Neurotransmitters are chemical messengers that carry signals between nerve cells, muscles, and glands. They are your body’s primary communication system.
Key neurotransmitters like serotonin and calcitonin gene related peptide (CGRP) have been found at abnormal levels in individuals during migraine attacks.[12]
If chemical messengers are out of balance, they can cause blood vessel “traffic jams” in the form of excessive inflammation[13], as well as the direct transmission of pain signals like migraine[14]. The exact neurochemical pathways are complex, involving various triggers and responses that make migraines highly individual and sometimes unpredictable.
- During the fight-or-flight “stress” response, the body creates a surge in chemical neurotransmitter hormones like adrenaline and noradrenaline, resulting in elevated levels in the brain.[16,17] These hormone-chemicals help produce increased heart rate, blood pressure, and energy mobilization, while also enhancing alertness and muscle readiness.
- In the opposing “rest & digest” response, the body increases the release of chemicals like acetylcholine, which promotes relaxation, decreases heart rate and blood pressure, and enhances digestion and metabolic processes.
- As a reaction to pain, the body releases pain-relieving chemical-hormones called endorphins.
Hormones and chemicals in the brain can self-regulate dramatically, which directly places physical pressures and shifts chemistry in the very same TGVS area that is associated with migraines. For example, when the body boosts heart rate and blood pressure during “fight or flight,” it does so by dilating the blood vessels in the brain.[18] This causes real physical pressure changes in the brain, along with possible migraine headaches.
Your cells are constantly working to solve & prevent your migraine
In order to learn how to reduce the severity of your migraines, it’s important to understand that your cells are working at full capacity to prevent debilitation from migraines. Well, to be clear, they are working at “full” capacity so long as:
- You do not have other internal issues occurring that your body deems more serious than a migraine.
- You have enough resources to allocate to manage the chemical & pressure changes that cause migraine.
If you take one thing from this article, let it be this:
You can help your cells do a better job of managing their internal chemistry by giving them every bit of health-enhancement possible (and simultaneously removing as many health-detriments as possible).
Nerve Cells
Your nerves, including the ones located in the TGVS, are made of nerve cells, which are called neurons. Electrical signals pass from one nerve cell to another. But in order to do this, neurotransmitter chemicals must be released from the end of one nerve cell. (These are the same internal chemicals we’ve been talking about above!) The neurotransmitter chemicals travel across the gap (the synapse) between cells, and must then successfully attach to the other nerve cell.
The amount of mechanical and chemical precision – that most of us take for granted – is extraordinary. This chemical movement is what causes “electricity” to move along your nerve cells.

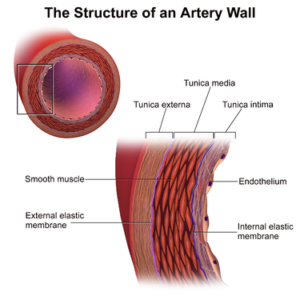
Blood Vessel Cells
Meanwhile, your blood vessels, including the ones located in the TGVS, are also made from cells like the following:
- Endothelial Cells – These are cells that form the inner lining of blood vessels. They naturally form a barrier between the blood and the rest of the inner vessel wall. They affect blood pressure by sending chemical signals that tell the smooth muscle cells to contract or not.[20] These are paracrine signaling molecules like nitric oxide (NO) and prostacyclin.[21]
- Smooth muscle Cells – These cells make up the middle layer of most blood vessels. As a muscle, they are able to contract & relax to control the size of the blood vessel. Smooth muscle cells are the mechanical structures that either apply pressure, or release pressure, from the blood flowing through the vessels.
Fibroblast Cells – Fibroblasts ensure structural support and integrity to various tissues. Beyond their foundational role in maintaining tissue architecture, fibroblasts are dynamic in their response to injury and inflammation: they can transition into a more active state, secreting cytokines and growth factors that influence immune responses and wound healing.[22] In pathological conditions, including neurogenic inflammation associated with migraine, fibroblasts interact chemically with immune cells and nerves, potentially exacerbating or modulating inflammatory and pain processes.[23] Their ability to affect the surrounding cellular environment and contribute to inflammatory states highlights their multifaceted role in both health and disease.
Diverse Cells of the Meninges Membranes
At the same time as the nerves and blood vessel cells are spouting their molecular chemistry, the three membrane layers of meninges that line your skull have their own chemical reactions. These membranes (the dura mater, arachnoid, and pia mater) line the skull and enclose the brain. They form a layer of protection for the brain, the outer layer of the blood-brain barrier.[25]
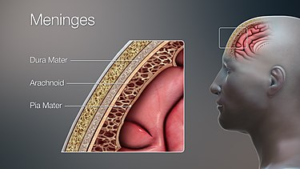
These chemical reactions are attempting to change the amount of fluid that can get through the blood-brain barrier, in attempts to protect against pathogen entry.
Furthermore, these chemical mediators can recruit additional immune cells from the bloodstream to the site of infection, enhancing the defensive response.[30] Research indicates that brain cells like astrocytes and microglia can produce and release antimicrobial peptides, including β-defensins, contributing to the brain’s innate immune response.[31]
How is the homeostasis in your brain?
Taken together, these coordinated chemical and cellular defense mechanisms are vital for maintaining the homeostasis around your brain.
Can you get a sense for how delicate and precise the chemical reactions must be in order to maintain homeostasis in the TGVS? Can you get a sense for how this has made it difficult for scientists to identify precisely just one cause of migraine?
What could be attacking your brain?
Pain is your body’s communication that something is off. Pain can be triggered by various types of damage, such as physical, heat-related, or molecular.

A pain receptor is called a nociceptor. Not all cells have pain receptors. Although the brain itself lacks nociceptors, these pain receptors are present in the protective meninges tissues surrounding the brain. “Chemicals released from blood vessels near the dura and pia can activate nociceptors, resulting in headaches, such as migraines.”[32]
A nociceptor activates when it detects damaging stimuli, which can be mechanical, thermal, or chemical.[33] This activation triggers ion channels on the nociceptors membrane to open. The most significant of these are sodium (Na+) channels, whose opening allows sodium ions to flow into the neuron. This alters the internal voltage of the nociceptor. If the voltage change is enough to reach a threshold, it generates an electrical signal.
This electrical signal travels along the nerve cells, utilizing neurotransmitters such as glutamate and substance P, to relay the pain message across synapses. The entire process involves a complex interplay of electrical impulses and neurochemical activity.
Why scientists don’t have a precise solution for migraines
What scientists seem to know about migraines is that they represent a lack of harmony within the nerves, connective tissues & blood vessels of the TGVS. The harmony of the cellular chemical interactions within the TGVS is somehow lost. And unfortunately, the sheer amount of possible chemical disruptions make it difficult for scientists to pinpoint precise mechanisms for treating the migraine pain.
Optimally functioning nerve & blood vessel cells means that the cells are able to coordinate their various chemicals in harmony. This streamlines all of your body functions. And this is true of all cells in your body, really all day long, not just inside the delicate balance of your TGVS.
While one person’s chemical disharmony may manifest as a migraine, another person’s genetic predisposition may be toward potentially any other recurring health condition, like diverticulitis or arthritis.
When it comes to migraines, it helps to do everything possible to make sure that we are striving to enhance the harmonious chemical regulation within our TGVS. In the murky world of migraines, bolstering our innate healing mechanisms should be a priority.
Pregnancy effects on Migraines
Pregnancy is a time of massive internal changes to both chemistry (via nerves & hormones) and physiology (blood vessels & pressure). These massive fluctuations can either stop or start migraines, and more than half of women with migraines actually report improvement during pregnancy.[34,35]
If aura – the visual disturbances that can precede migraine attacks – is not present in your usual migraines, pregnancy is especially likely to reduce the frequency and severity of attacks![36]

Specifically, studies show that varying levels of ovarian hormones, especially estrogen, influence serotonin and CGFP levels, making women predisposed to migraine headaches, even during monthly menstrual cycles.[40]
The initial pregnancy-related priority when presenting with a migraine for the first time is to identify whether it is being triggered by something potentially more dangerous, like preeclampsia or cerebral venous thrombosis[41] (your childbirth guides should be able to help you rule these out).
Different studies show the effect of breastfeeding on the postpartum occurrence of migraine to be less impactful than pregnancy,[42] although somewhat unclear.[43]
5 Foundational Health Measures for Migraine Reduction
If your internal chemistry is overwhelmed or otherwise discombobulated, the most important first step is to make sure that you’ve taken every step toward supporting your internal chemical balance. That involves the 5 Foundations of Health & Wellbeing:
- ONE: 3 Ways that Diaphragmatic Breathing can reduce migraines
- TWO: 5 Ways that Intense Exercise can reduce migraines
- THREE: 3 Natural Nutrition ways to reduce migraines
- FOUR: 3 Ways that Sound Sleep can reduce migraines
- FIVE: Stress Management can reduce migraines
ONE: 3 ways that Diaphragmatic Breathing can reduce migraines
Tens of thousands of times per day, you send a stimulus for your body to lean either toward or away from the chemistry of “fight of flight.” This lean directly impacts blood vessel dilation, as well as internal pH balance that can affect all cellular function, including in the TGVS.
Here are 3 ways that proper diaphragmatic breathing, all throughout the day, may be able to prevent your migraine:
- Stress reduction – Every breath you take shifts you either slightly toward fight or flight (if you’re a classic “chest breather”) or “rest & digest” (if you are a natural torso breather. That’s literally every breath you take, that you have an opportunity to nudge your internal chemistry toward or away from the “stress-related” causes of migraine.
- Oxygenation – Enhanced blood oxygenation helps stabilize the function of the trigeminovascular system, potentially mitigating migraine triggers related to vascular issues.[44]
- Detoxification – Proper breathing facilitates better lymphatic drainage and removal of toxins from the body. Since the buildup of toxins can contribute to the onset of migraines, improved detoxification can help in reducing their frequency.[45]
Most people need to be literally taught how to breathe correctly, and given a program to practice daily to incorporate breathing. (Go here for a single session breathing assessment, and to receive a 5-minute daily exercise breathing plan).

TWO: 5 Ways that Intense Exercise can reduce migraines
Intense strength training as well as intense cardiovascular training are both scientifically validated to cause the most epigenetic longevity chemistry changes that we know today. Exercise is literally your direct access to coaching your chemistry to perform more optimally. Intensity is important to help you move from your current set point of chemistry creation to something new. Exercise also helps carve the cellular circadian rhythms that not only help with sleep at night, but also with the chemical exchanges all throughout the day.
Here are 5 ways that exercise can directly prevent migraines:
- Endorphins – Physical activity stimulates the production of endorphins, natural painkillers.
- Blood vessel health – Regular exercise promotes better blood flow and vascular health, which can stabilize changes in blood vessel diameter that contribute to migraine attacks. This stabilization might help reduce the frequency or intensity of migraines by preventing abnormal vasoconstriction and dilation that are part of the migraine process.
- Serotonin – Exercise can increase serotonin levels in the brain, which helps regulate mood and pain. Since fluctuations in serotonin are linked with the initiation of migraine attacks, stabilizing its levels through exercise may provide a preventative benefit.
- Stress management – Exercise is a well-known stress reliever. Since stress is a common trigger for migraines, reducing stress through regular physical activity might decrease the frequency of migraine episodes by lessening the sympathetic nervous system’s activation, which impacts the TGVS.
- Inflammation – Inflammation increases the excitability of the trigeminal neurons in the TGVS. Increased physical activity reduces systemic inflammation,[46] thereby reducing the hypersensitivity of the nerve that transfers the pain signals.
(See Epigenetic Phenomena in Pregnancy to see 4 specific examples of how exercise stimulates epigenetic chemical changes that affect your body and your baby.)

THREE: 3 Natural Nutrition ways to reduce migraines
Do these three Natural Nutrition action steps, as well as you can:
The first thing to do with your nutrition is to remove artificial ingredients. Remove the molecules that could be directly attacking your internal chemical balance. This means you may need to read food labels, and generally aim to eat foods that you can pronounce, avoiding the ingredients that sound like chemicals. Start by removing ingredients that others have already discovered to be connected with migraines (like aspartame, MSG, artificial colors, nitrates/nitrites, and sulfites). Then, realizing that our food protection agencies cannot keep up with the introduction of new food chemicals, remove others that could be the cause. Replace these foods with more natural whole food ingredients.
The next step is to remove processed carbohydrates that cause insulin & blood sugar swings. Removing processed carbohydrates will reduce your chances of:
-
- Blood vessel reactivity – This is sugar molecule binding along blood vessel walls that impairs your blood vessels ability to dilate and constrict properly, directly affecting migraine status.
- Inflammation – Inflammation is a well-known trigger of migraine. Elevated glucose levels increase the production of pro-inflammatory cytokines and oxidative stress, further irritating the meningeal tissues and trigeminal nerve endings.
- Insulin resistance – Insulin resistance promotes endothelial dysfunction (remember the inner lining of the blood vessels?!). We need to make sure that those cells function properly, in order to avoid migraine.
- Glucose fluctuations – The classic blood sugar swings that come from processed carbohydrate foods can affect serotonin levels, which significantly affect migraines. Low blood sugar is linked with decreased serotonin. When serotonin levels drop, it can dilate blood vessels that affect migraine pain.
After that, remove processed foods, in general – and replace them with natural whole food, vegetable and animal foods – so that you can make it easy for your body to create the chemical building blocks that can work in harmony. You are what you eat. Try giving your internal systems every possible advantage for harmonious function.

FOUR: 3 Ways that Sound Sleep can reduce migraines
Your internal chemistry works better when you go to bed and wake up at the same time every day. Also, “nighttime hormones” are more likely to be produced at the right times when you avoid screens after dark, and sleep in as close to pitch-black as you can. Remember, you want to work with your natural evolutionary cycles, not against them. Going to bed with the sun, and without turning on light bulbs, is what got humanity to where we are today.
Here are 3 specific ways that sleep can affect your migraines:
- Inflammation, Hormones & Neurotransmitters – Sleep is the greatest inflammation reducer, and hormone & neurotransmitter regulator! Poor sleep can increase pro-inflammatory substances and hurt serotonin & dopamine levels. Sleep also affects your regulation of cortisol and melatonin, which are involved in regulating pain and blood vessel dilation.[47,48,49,50] Disrupted sleep patterns can lead to imbalances in these hormones, contributing to migraine triggers or exacerbation.
- Reduction of Cortical Spreading Depression (CSD) – Sleep is believed to protect against CSD, a wave of neural and glial[51] depolarization thought to underlie the aura phase of migraine in some individuals.[52]
- Stress-management – The most profound way to balance your “fight or flight” and “rest & digest” chemistry is to make sure that you have enough rest to do so. “Stress” is a well-known trigger for migraines, and good quality sleep is effective in reducing stress.

FIVE: Stress Management can reduce migraines
You are a chemical factory. There are two options: “fight or flight,” and “rest & digest.” In all of its many forms, “stress” is a trigger for migraines. Where can you further reduce stress in your life right now?
Reducing stress can be anything from a formal routine of prayer & meditation to just simply not packing your schedule so full. It could mean taking time with friends once per week, or completely changing your job to something you’re more passionate about.
You are a unique individual, and if you’re going to solve your migraines, you may need to get to know yourself in a deeper way.
If it’s not already obvious at this point in this long & comprehensive article about migraine reduction, the chemistry underlying stress dramatically affects whether you have a migraine, and how severe it is. In fact, all of the other natural solutions for migraine include some form of “stress reduction.”
Good breathing, exercise, nutrition and sleep all reduce stress. And it’s also true that stress reduction helps you to breathe better, exercise better, eat better, and sleep better.

What to record in your migraine journal
A starting step that is often recommended for migraine management is keeping a daily journal. Things to record in your journal include:
- When you have a migraine
- Notes about each of the 5 foundations above (when you exercise, what you ate, the time you went to bed, your perceived level of stress in the day, and how much you were present with your breathing in the day).
If you haven’t kept a journal already, start one now, and do it long enough until you see the pattern emerge.
As you do this, note also that while migraines are ultimately chemical-based, there are some tension headaches that can have a very simple mechanical fix. If you wonder about this, consider performing some sort of myofascial relaxation on the muscles of your neck and upper back / shoulders every day for a while, to see if this mechanically helps reduce the tension of these muscles. (Other exercises can be performed for posture strengthening too – consider getting a corrective exercise assessment to learn which muscles are over-active in you, and how to turn them off.)
Blending Therapies as you work on the true cause of migraines
Internal chemistry is at the source of migraine pain, and there are multiple ways to address that chemical balance. In order to solve the true cause, you will need to address your chemistry and the best way to do this is at the source: your internal chemical factory: Breathing, Exercise, Nutrition, Sleep, and the mindfulness of Stress Reduction.
However, we know how incredibly debilitating and frustrating migraines are, and you should know that some people do find relief from: supplements, pharmaceutical drugs, and even surgery. Although these are beyond the scope of this article, here are just a couple bullet points to help you on your way:
Supplements & Herbs show inconsistency for migraines
- 2010 Study: “Among ‘natural’ treatments, both butterbur extract and vitamin B2 have shown efficacy in more than one randomized trial and are thus potentially useful first-line preventive interventions.”[53]
- 2020 Study: “There were positive, preliminary findings on curcumin, citron, and coriander as a prophylactic [preventative] treatment for migraine, and the use of menthol and chamomile as an acute treatment. However, the risk of bias was high for many studies.”[54]
Pharmaceutical drugs show mixed results for migraines
- 2017 Study: “Unfortunately, less than 50% of patients taking oral triptans are pain-free at 2 hours, and 30% have a reoccurrence of headache within 24 hours… Although they are the only drugs specifically developed to treat migraine headache, the exact mechanism by which triptans reduce migraine pain is unknown.”[55]
- Triptans are a group of medicines used to treat migraine
- 2020 Study: “Although a number of drugs have been used for treatment of migraine, most of these are not effective for every patient and may have undesirable side-effects. Thus, there is an enormous unmet need in current migraine therapy for discovering safer and more effective agents.”[56]
Injections & Surgery help some with migraines
- 2020 Study: Botox injection: “Migraines headaches often are refractory to medical therapy and may respond well to botulinum toxin type A.”[57]
- 2020 Study: “Migraine surgery is another option to release trigger sites. A systematic review of the migraine surgery literature found an average success rate of 90%, with elimination or greater than 50% improvement of migraine headaches after migraine surgery.”[58]
If you’d like any particular help understanding any of these additional therapies, please feel free to email us your specific questions.
—————————–
If you would like fun & research-based guidance as a fitness professional, or during your own pregnancy & postpartum, please check out these Fit For Birth offerings:
- Fitness & Wellness Professionals:
- FREE 1-hour CEC
- CEC/CEU Courses, including our Pre & Postnatal Corrective Exercise Specialist (PPCES), the world’s first holistic perinatal CEC/CEU!
- Monthly Elite Membership – Community. Monthly education. Business mentorship & work opportunities. $27/month.
- Pregnancy, Pre-conception & Postpartum:
—————————————————-
James Goodlatte is a Father, Holistic Health Coach, Corrective Exercise Practitioner, Speaker, Author, Professional Educator, and the founder of Fit For Birth and Exercise For Longevity. Since 2008, when he found out he would be a father, his passion for holistic wellness shifted to children and families. Today, he is a driving force in providing Continuing Education Credits for the pre and postnatal world, with Fit For Birth professionals in 52 countries. James is a contributing member of the First 1000 Days Initiative at the Global Wellness Institute, and longevity researcher & educator.
References
[1] 2017. Jacobs, Blaine. Dussor, Gregory. Neurovascular contributions to migraine: moving beyond vasodilation. Neuroscience. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC5083225/
[2] 2018. Jarvis, et al. Managing Migraine in Pregnancy. BMJ. Retrieved 11/10/24 from https://www.bmj.com/content/360/bmj.k80.full
[3] 2003. Pietrobon, Daniela. Striessnig, Jorg. Neurobiology of migraine. Nature Reviews Neuroscience. Retrieved 11/10/24 from https://www.nature.com/articles/nrn1102
[4] 2012. Waite, Phil M.E.; Ashwell, Ken W.S. Trigeminal Sensory System. The Human Nervous System (Third Edition). Retrieved 11/10/24 from https://www.sciencedirect.com/topics/neuroscience/trigeminovascular-system
[5] 2024 [last updated]. Huff, et al. Neuroanatomy, Cranial Nerve 5 (Trigeminal). StatPearls [Internet]. Retrieved 11/12/24 from https://www.ncbi.nlm.nih.gov/books/NBK482283/
[6] Image: [n.d.] Slideshare. Retrieved 11/10/24 from https://www.slideshare.net/slideshow/trigeminovascular-system-seminar/42013448
[7] 2017. Jacobs, Blaine. Dussor, Gregory. Neurovascular contributions to migraine: moving beyond vasodilation. Neuroscience. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC5083225/
[8] 2016. Malhotra, Rakesh. Understanding migraine: Potential role of neurogenic inflammation. Annals of Indian Academy of Neurology. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC4888678/ “In particular, it has become increasingly evident that the activation of meningeal afferents, neuropeptide release, and neurogenic inflammation plays a pivotal role in the generation of pain in migraine headache.”
[9] [n.d.] Environmental & Physical Factors. National Headache Foundation. Retrieved 11/10/24 from https://headaches.org/environmental-factors/
[10] 2024. Gotter, Ana. 9 Foods that trigger migraine (and alternatives). Healthline. Retrieved 11/12/24 from https://www.healthline.com/health/foods-that-trigger-migraines
[11] 2016. Gonzalez, et al. Migraines Are Correlated with Higher Levels of Nitrate-, Nitrite-, and Nitric Oxide-Reducing Oral Microbes in the American Gut Project Cohort. mSystems – American Society for Microbiology. Retrieved 11/12/24 from https://pubmed.ncbi.nlm.nih.gov/27822557/
[12] 2012. Aggarwal, et al. Serotonin and CGRP in Migraine. Annals of Neurosciences. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC4117050/
[13] 2021. Kursun, et al. Migraine and neuroinflammation: the inflammasome perspective. The Journal of Headache and Pain. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC8192049/ “A recent review suggested that D-β-hydroxybutyrate (D-BHB), one of ketone bodies, is implicated in migraine pathophysiology, that is in mitochondrial function, oxidative stress, cerebral excitability, inflammation…”
[14] 2023. O’Hare, et al. Excitation-Inhibition Imbalance in Migraine: From neurotransmitters to Oscillations. International Journal of Molecular Sciences. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC10299141/ “There may be excessive glutamate but reduced GABA levels in migraine” “Taken together, there is evidence of an imbalance between excitation and inhibition in migraine.”
[15] Image: Nava Health. Retrieved 11/12/24 from https://navacenter.com/brain-chemistry-panel/
[16] 2024 [last update]. Chu, et al. Physiology, Stress Reaction. StatPearls [Internet]. Retrieved 11/10/24 from https://www.ncbi.nlm.nih.gov/books/NBK541120/
[17] [n.d.] Norepinephrine (Noradrenaline) Cleveland Clinic. Retrieved 11/10/24 from https://my.clevelandclinic.org/health/articles/22610-norepinephrine-noradrenaline
[18] 2015. Gordon, et al. Autonomic and endocrine control of cardiovascular function. World Journal of Cardiology. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC4404375/ “Importantly, epinephrine serves to initiate the fight or flight response system by boosting the oxygen and glucose supplies to the brain and skeletal muscle through increased cardiac output and vasodilatation.”
[19] Image: 2024. BNO Team. Neuron – Definition, Structure, Types, Functions. Biology Notes Online. Retrieved 11/10/24 from https://biologynotesonline.com/neuron-definition-structure-types-functions/#google_vignette
[20] 2019. Wilson, et al. Increased Vascular Contractility in Hypertension Results From Impaired Endothelial Calcium Signaling. Hypertension. Retrieved 11/10/24 from https://physoc.onlinelibrary.wiley.com/doi/pdf/10.1113/expphysiol.2007.038588
[21] 2007. Mitchell, et al. Role of nitric oxide and prostacyclin as vasoactive hormones released by the endothelium. Experimental Physiology – Symposium Report. Retrieved 11/12/24 from https://pubmed.ncbi.nlm.nih.gov/17965142/
[22] 2022. Cialdai, et al. Role of fibroblasts in wound healing and tissue remodeling on earth and in space. Frontiers in Bioengineering and Biotechnology. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC9578548/
[23] 2024. Levy, Dan. Moskowitz, Michael. Meningeal Mechanisms and the Migraine Connection. Annual Review of Neuroscience. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC11412714/ “Released tryptases activate protease-activated receptor-2 (PAR2), expressed by meningeal afferents and fibroblasts.” (Tryptase is an immune protein)
[24] Image: Wikipedia: Retrieved 11/12/24 from https://en.wikipedia.org/wiki/Tunica_intima
[25] 2020. Turtzo, et al. Meningeal blood–brain barrier disruption in acute traumatic brain injury. Brain Communications. Retrieved 11/12/24 from https://academic.oup.com/braincomms/article/2/2/fcaa143/5903386
[26] Image: Meninges. Wikipedia. Retrieved 11/12/24 from https://en.wikipedia.org/wiki/Meninges
[27] 2023. Levy, Dan. Moskowitz, Michael. Meningeal Mechanisms and the Migraine Connection. Annual Review of Neuroscience. Retrieved 11/12/24 from chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://www.annualreviews.org/deliver/fulltext/neuro/46/1/annurev-neuro-080422-105509.pdf?itemId=/content/journals/10.1146/annurev-neuro-080422-105509&mimeType=application/pdf
[28] 2018. Rua, Rejane. McGavern, Dorian. Advances in Meningeal Immunity. Elsevier. NIH. Retrieved 11/12/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC6044730/ “Mast cells reside in the dura mater and can be activated by release of alarmins from damaged cells or in response to meningeal nerve activity.”
[29] 2023. Zhang, et al. Role of neuroinflammation in neurodegeneration development. Signal Transduction and Targeted Therapy. Retrieved 11/12/24 from https://www.nature.com/articles/s41392-023-01486-5
[30] 2024. Rebejac, et al. Role of meningeal immunity in brain function and protection against pathogens. Journal of Inflammation. Retrieved 11/12/24 from https://journal-inflammation.biomedcentral.com/articles/10.1186/s12950-023-00374-7
[31] Retrieved 11/12/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC3346844/
[32] 2014. Basbaum, Allan. If the brain can’t feel pain, why do I get headaches? BrainFacts. Retrieved 11/12/24 from https://www.brainfacts.org/ask-an-expert/if-the-brain-cant-feel-pain-why-do-i-get-headaches
[33] 2022. Gore, David. The anatomy of pain. Anaesthesia & Intensive Care Medicine. Retrieved 11/12/24 from https://www.sciencedirect.com/topics/medicine-and-dentistry/nociceptor
[34] 2016. Wells, et al. Managing Migraine During Pregnancy and Lactation. Current Neurology and Neuroscience Reports. Retrieved 11/10/24 from https://link.springer.com/article/10.1007/s11910-016-0634-9
[35] 2018. Jarvis, et al. Managing Migraine in Pregnancy. BMJ. Retrieved 11/10/24 from https://www.bmj.com/content/360/bmj.k80.full
[36] 2008. Goadsvy, et al. Migraine in Pregnancy. BMJ. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC2440903
[37] Image: American Pregnancy Association. Retrieved 11/12/24 from https://americanpregnancy.org/healthy-pregnancy/pregnancy-health-wellness/headaches-and-pregnancy/
[38] 2016. Wells, et al. Managing Migraine During Pregnancy and Lactation. Current Neurology and Neuroscience Reports. Retrieved 11/10/24 from https://link.springer.com/article/10.1007/s11910-016-0634-9
[39] 2008. Goadsvy, et al. Migraine in Pregnancy. BMJ. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC2440903
[40] 2012. Aggarwal, et al. Serotonin and CGRP in Migraine. Annals of Neurosciences. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC4117050/
[41] Cerebral venous thrombosis (CVT) is a rare but serious condition that occurs when a blood clot forms in the brain’s veins or sinuses, blocking blood flow.
[42] 2019. Burch, Rebecca, MD. Epidemiology and Treatment of Menstrual Migraine and Migraine During Pregnancy and Lactation: A Narrative Review. Headache: The Journal of Head and Face Pain. Retrieved 11/10/24 from https://doi.org/10.1111/head.13665
[43] 2016. Wells, et al. Managing Migraine During Pregnancy and Lactation. Current Neurology and Neuroscience Reports. Retrieved 11/10/24 from https://link.springer.com/article/10.1007/s11910-016-0634-9
[44] 2019. Iyengar, et al. CGRP and the Trigeminal System in Migraine. Headache. Retrieved 11/12/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC6593989/
[45] 2023. Morgan, Kendall. Lymph Drainage Massage: Benefits and Risks. WebMD. Retrieved 11/12/24 from https://www.webmd.com/a-to-z-guides/what-is-lymph-drainage-massage
[46] 2011. Gleeson, et al. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nature Reviews Immunology. Retrieved 11/12/24 from https://www.nature.com/articles/nri3041
[47] 2010. Cook, et al. Melatonin differentially affects vascular blood flow in humans. American Journal of Physiology: Heart and Circulatory Physiology. Retrieved 11/13/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC3044053/
[48] 2016. Emet, et al. A Review of Melatonin, Its Receptors and Drugs. The Eurasian Journal of Medicine. Retrieved 11/13/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC4970552/
[49] 2005. Whitworth, et al. Cardiovascular Consequences of Cortisol Excess. Vascular Health and Risk Management. Retrieved 11/13/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC1993964/
[50] 2012. JC CHoi, MI Chung, YD Lee. Modulation of pain sensation by stress-related testosterone and cortisol. Association of Anaesthetists. Retrieved 11/13/24 from https://associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2044.2012.07267.x
[51] Glial cells: Cells that hold nerve cells in place
[52] 2017. O’Hare, M. Cowan, R.P. Sleep and Headache. Sleep and Neurologic Disease. Retrieved 11/12/24 from https://www.sciencedirect.com/topics/medicine-and-dentistry/cortical-spreading-depression
[53] 2010. Nicholson, et al. Nonpharmacologic Treatments for Migraine and Tension-Type Headache: How to Choose and When to Use. Neurology. Retrieved 11/10/24 from https://pubmed.ncbi.nlm.nih.gov/21080124/
[54] 2020. Lopresti, Adrian, et al. Herbal treatments for migraine: A systematic review of randomised-controlled studies. Phytotherapy Research. Retrieved 11/10/24 from https://pubmed.ncbi.nlm.nih.gov/32310327/
[55] 2017. Jacobs, Blaine. Dussor, Gregory. Neurovascular contributions to migraine: moving beyond vasodilation. Neuroscience. Retrieved 11/10/24 from https://pmc.ncbi.nlm.nih.gov/articles/PMC5083225/
[56] 2020. Tauchen, Jan. Natural Products and their (Semi-)Synthetic Forms in the Treatment of Migraine: History and Current Status. Current Medicinal Chemistry. Retrieved 11/10/24 from https://www.ingentaconnect.com/content/ben/cmc/2020/00000027/00000023/art00003
[57] 2020. Olla, et al. Migraine Treatment. Clinics in Plastic Surgery. Retrieved 11/10/24 from https://pubmed.ncbi.nlm.nih.gov/32115055/
[58] 2020. Olla, et al. Migraine Treatment. Clinics in Plastic Surgery. Retrieved 11/10/24 from https://pubmed.ncbi.nlm.nih.gov/32115055/
