Research-based and posted on April 21, 2021
If you haven’t yet read the first portion of this informational series, “What Abdominal Muscles Get Cut During a C-Section?”, consider visiting that article first.
Historical Background
“The first documented cesarean delivery (CD) was in 1020 AD. In 1882, the era of modern CD began when Saenger advocated closing all uterine incisions immediately after surgery. The lower uterine segment incision was introduced by Kronig in 1912 and popularized in the United States by DeLee in 1922. The transverse uterine incision was described by Munro-Kerr in 1926…Approximately 2 CDs are started every minute in the United States alone; this is the most frequent major operation that is performed in this country.”[1]
Overview of the Tissues that Get Cut during a C-Section
“To achieve a cesarean delivery, the surgeon must traverse all the layers that separate him/her from the fetus”:[2]
1. “First, the skin is incised, followed by the subcutaneous tissues.”
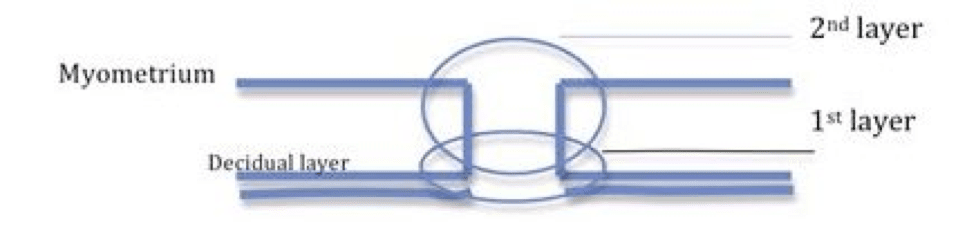
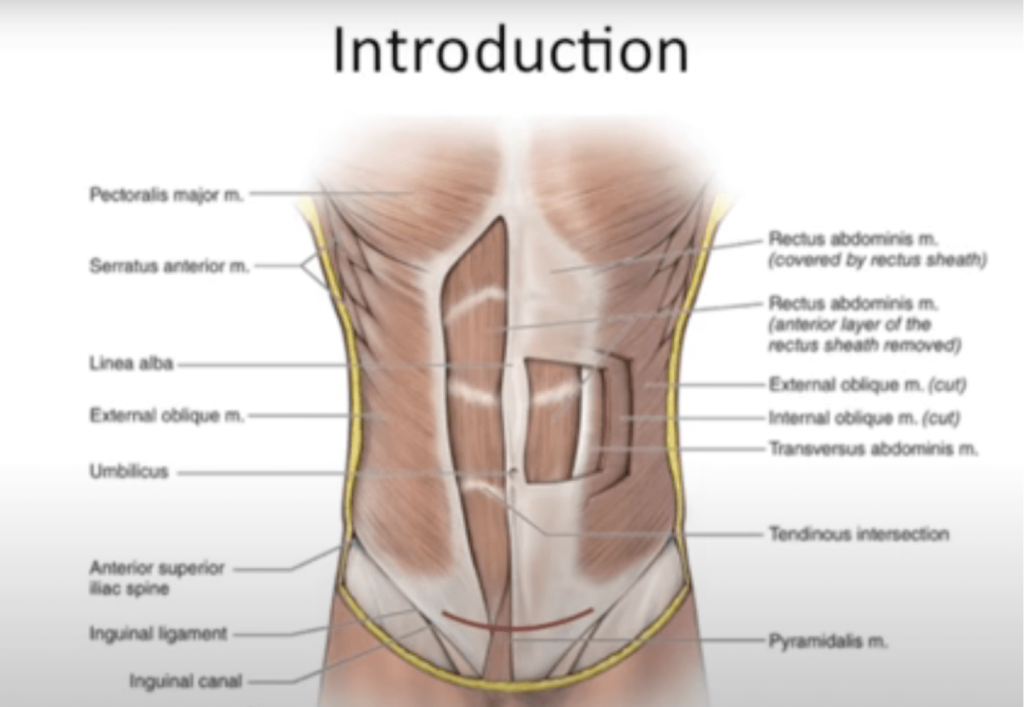
2. “The next layer is the fascia overlying the rectus abdominis muscles. The anterior abdominal fascia usually consists of two layers. One is composed of the aponeurosis from the external oblique rectus muscle, and the other is a fused layer which contains the aponeuroses of the transverse abdominis and internal oblique muscles.”
Fascia – a thin sheath of fibrous tissue enclosing a muscle or other organ
Aponeurosis – a sheet of fibrous tissue that takes the place of a tendon in flat muscles having a wide area of attachment
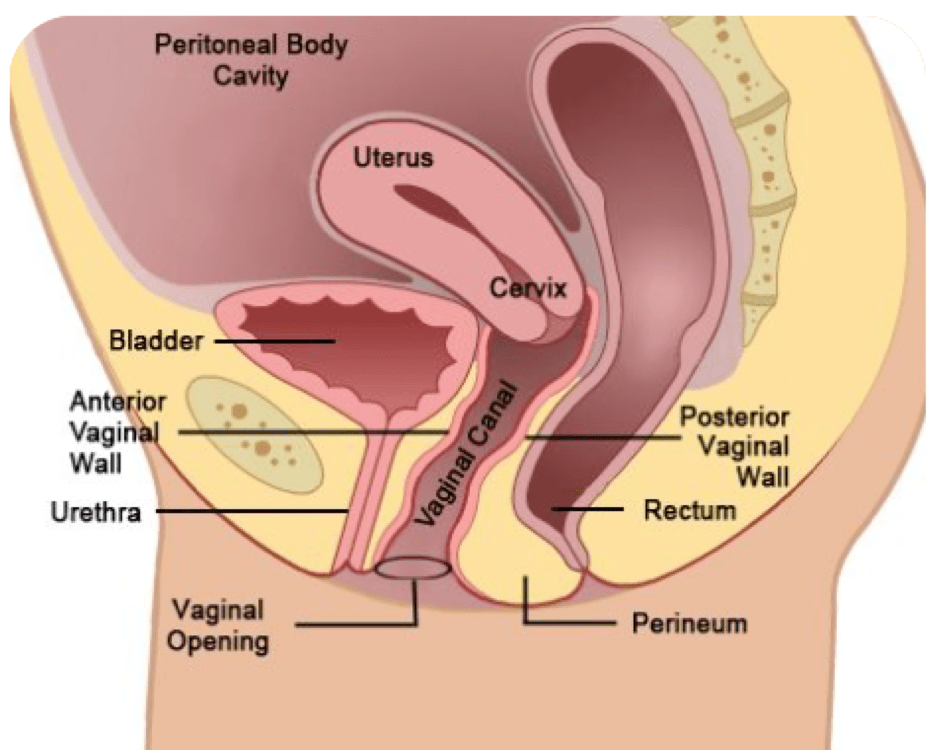
3. “After separating the rectus muscles…the surgeon enters the abdominal cavity through the parietal peritoneum.”
Peritoneum – membrane lining the cavity of the abdomen and covering the abdominal organs
4. “Depending on the status of the patient’s amniotic membranes (if her “water is broken” or intact), the surgeon could encounter that amniotic sac upon incision of the uterus…The amniotic sac, if present, would be the last layer between the surgeon and the fetus. It is at this point that the fetus is delivered, achieving the primary goal of the cesarean section.”
According to 2010 research in Gynecological Surgery, “At the most basic level, the only thing necessary is some cutting instrument. In an emergency, a physician could theoretically perform a perimortem cesarean delivery on a woman after a car accident with a sharp piece of glass.”[3] Equipment used can include: catheter running from the bladder, regional or general anesthesia, and a surgical tray that includes scissors, bandages, clamps, forceps, retractors, needle drivers and more.
The four main cesarean delivery techniques are:[4]
Pfannenstiel-Kerr – Pfannenstiel skin incision, followed by multiple sharp dissections (not blunt), closure of peritoneum, interrupted fascia closure, continuous skin suture.
Joel-Cohen – JC skin incision, followed by multiple blunt dissections, spontaneous placenta removal, non-closure of peritoneum
Misgav-Ladach – Same as JC (JC skin incision and blunt dissections), except: Misgav-Ladach uses manual placenta removal (not spontaneous), single layer running closure of the uterus (not interrupted), continuous closure of the fascia (not interrupted), mattress closure of the skin (not continuous)
Modified Misgav-Ladach – Pfannenstiel skin incision, followed by multiple blunt dissections, spontaneous placental removal, running uterine closure (not interrupted), closure of the peritoneum, continuous closure fascia closure, continuous skin suture.
Explanation of Closure/Sutures:
- Continuous/Running = single thread
- Interrupted = multiple small threads, one after the other